Volume : 1
Case Report
Correction of Deformities Around the Knee and Tibia Using Taylor Spatial Frame
M.Attia1, C.Whately2, T.Hadidi3, H. Barbary3, A. Zain3
1Specialist of Orthopedic Surgery at Cairo University&Emirates Hospital, Dubai
2Specialist of Orthopedic Surgery & Medical Director of MedCare Hospital, Dubai
3 Cairo University Hospital – Orthopedic Surgery Department.
Received: August 10, 2018 | Published: October 11, 2018
Abstract
The purpose of the study is to understand the basic principles of the Taylor spatial frame and to determine the effectiveness of the Taylor spatial frame for treatment of deformities around the knee and tibia in pediatric and adolescent patients.
Design
Prospective
Setting
25% of the patients had their operations in Cairo university hospitals while 75% had their operations in the American and Medcare hospitals Dubai.
Patients:
20 limbs in 16 patients. The femoral deformities were 3 valgus associated with rotational deformities in the distal femurs. 3 varus deformity distal femur, and one shortened limb. The tibial deformities were 5 varus proximal tibias, 3 external rotation deformities, one valgus ankle, one varus ankle, one recurvatum proximal tibia and one valgus proximal and distal tibia.
Inclusion criteria:
The patients that in need of any gradual deformity correction around the knee and tibia. Patients with uni or multiplaner frontal plane deformity, sagittal plane deformities, presence of rotational deformity within the target age group (6-18 years) are included.
Exclusion criteria:
Patients with uniplanar frontal plane deformity less than 10 degrees or any case with acute intraoperative correction of the deformity are excludedcorrection of the deformities by using Taylor Spatial Frame after a precise preoperative planning and introducing the deformity and frame mounting parameters to the web based Taylor Spatial Frame software program to generate correction schedules.
Main Outcome Measurements:
Alignment of the lower limb after frame removal and at the time of the final follow up assessed radio-logically using mechanical axis deviation test and clinically using the Association for the study of the method of Ilizarov (ASAMI) bone and functional scores. Time and accuracy of the correction. Functional outcome, and complication rate.
Results:
The mean time in frame was 5.8 months (range, 2–11 months). Frontal and sagittal plane deformities were corrected to within normal values. The frame was used dynamically to correct all deformity for a mean time of 4.85 weeks (range, 2–11weeks). Our deformities were reduced from a mean of 25° (range from 10-60°) preoperatively to a mean of 3° (range from 1-7°) at the latest follow up. The mean lengthening was 2.8 cm (range from 1.5-5cm).
Conclusions:
Based on our results, we believe the TSF allows safe correction of distal femoral and tibial deformities in children and young adults. It is accurate especially in multiplanar deformities with a complication rate that is well tolerated.
Introduction
Distal Femoral and tibial deformities can be corrected by several methods, including Hemiepiphysiodesis, Osteotomy and internal fixation or an osteotomy and external fixation. An acute or gradual correction could be obtained with either a monolateral or a circular fixator. But proper preoperative planning of the deformity and how to determine the site of the osteotomy is very important for correction.1
Feldman et al. reported that gradual correction was more accurate than acute correction in the treatment of tibia vara.2The Ilizarov circular external fixator uses multiple components, each designed to address specific planar deformities (translation, rotation, or angulation) to gradually correct limb deformities, even complex ones.3
The Ilizarov device, despite its capabilities, requires extensive planning for building a frame to correct angulation, translation, and rotation simultaneously. Additionally, building the frame and making revisions to correct residual deformities are often difficult and labor intensive.2
In attempts to overcome these limitations of the Ilizarov device, The TSF is an alternative circular external fixator with rings, bolts, nuts, and attachments similar to those of the Ilizarov, but uses a hexapod-like arrangement of six telescopic struts and special universal joints for attaching the two rings together. The accompanying computer software provides the TSF with the advantage of permitting the gradual correction of a multiaxial deformity across all planes simultaneously and correction of any residual deformity without changing the mounted frame.4
The accuracy of the TSF versus the Ilizarov ring fixator (IRF) was evaluated in a study by Manner et al. Who compared the final result after frame removal with the Initial aim of deformity correction and lengthening. A total of 278 consecutive lower-limb deformity corrections treated either with the TSF or IRF were evaluated. Of the 79 cases treated with the IRF, there was no residual deformity in 44 cases (55.7%). Of the 129 cases treated with TSF, there was no residual deformity in 117 cases (90.7%). In both groups, one essential finding was obvious. With rising dimensions of axial corrections, an increasing percentage of residual deformities could be seen. The goal of treatment in one-dimensional corrections was achieved in 79.3% of the IRF cases and in 100% of the TSF cases; similarly, in two-dimensional corrections, the goal of treatment was achieved in 48.6% of the IRF cases and in 91.8% of the TSF cases, while in three-dimensional corrections it occurred in 28.6% of the IRF cases and 91.1% of the TSF cases. And lastly, in four-dimensional corrections the goal was not achieved in the IRF case but in 66.7% of the TSF cases. In conclusion, their study showed clear advantages of the TSF compared to the Ilizarov ring fixator in complex multiplanar deformities.4
Patients and Methods
From March 2011 to October 2013, a prospective study was undertaken to evaluate the effectiveness of TSF in the correction of deformities around the knee and the tibia. 20 limbs in 16 patients were operated upon; all patients were followed up for a mean of 8 months (range: 1-16 months). Patients had their operations in Cairo University Hospital and Medcare Hospital Dubai.
Patients age range between 6–18 years old at the time of surgery. The mean age was 13.6 years. 37.5 % of our patients were females (6 female and 10 male).Operations were performed on 8 femurs and 12 tibias, 5 were left side and 9 were right side and 3 is bilateral.
Indications for surgery:
The etiologies of the femoral deformities were one post traumatic, 4 developmental (idiopathic) and two Metaphyseal Dysplasia.
The femoral deformities were 3 valgus deformity distal femurs associated with rotational deformity, 3 varus deformity distal femurs, and one shortened limb.
The etiologies of the tibial deformities were one Blount’s disease, 2 congenital psuedoarthrosis and 7 developmental (idiopathic). The tibial deformities were 5 varus proximal tibias, 3 external rotation deformities, one valgus ankle, one varus ankle, one recurvatum proximal tibia and one valgus proximal and distal tibia.
All the patients were evaluated for: A. fitness for surgery. B. musculoskeletal evaluation being subjected preoperatively to a through history taking and physical examination. The patients were evaluated clinically and radiological both preoperatively and postoperatively.
A- Clinical assessment: Results are assessed using Association for the Study and Application of the Method of ILIZAROV (ASAMI) bone and functional scoring system.
Radiographic Assessment: Every deformity was analyzed for translation and/or angulation in the frontal, sagittal, and axial planes, resulting in a total of six axes. Both preoperative and postoperative radiographs are available for all the limbs.
1-Full-length standing A-P and lateral radiographs.
Frontal and saggital plane deformity is measured on a standing long radiograph. Key variables included MAD (Mechanical axis deviation) which is determined with use of the malalignment test and joint orientation angles, the mechanical lateral distal femoral angle (mLDFA) and posterior distal femoral angle (PDFA) are measured for distal femoral deformities, medial proximal tibial angle (MPTA), posterior proximal tibial angle (PPTA) are measured for proximal tibial deformities, and lateral distal tibial angle (LDTA) and anterior distal tibial angle (aADTA) are measured for distal tibial deformities. All angles were measured using the methods described by Paley et al.5 (5)
The center of rotation of angulation is identified by locating the intersection of the proximal and distal mechanical axes. Accuracy was measured with the radiographic angles either being brought to the normal range or not. If there was a leg-length discrepancy (LLD), blocks (to the nearest 5 mm) were placed under the affected foot to level the pelvis and the height of the blocks was recorded. LLD was measured on the radiograph
2-C.T scan
Rotational deformity was measured clinically by observing gait, foot progression angle, and thigh-foot axis in the prone position. A CT version study of the Femur and tibia was performed in cases with clinically obvious deformity to measure the amount of axial angulations (internal/external rotation of the femur or tibia). This is a simple method to evaluate the correct rotational profile objectively. It involves taking serial computed tomography cuts through the femoral neck, femoral condyle, tibial plateau and tibial plafond while the limb is held in position. The angle between femoral neck and the transverse axis of femoral condyle gives the correct rotation of femur. The angle between the tibial plateau and plafond gives correct rotation of the tibia
Surgical Data
Operating-Room Setup
The patient is taken to the operating room and placed supine on a radiolucent operating table. Sheets are placed under the ipsilateral hip to internally rotate the lower extremity until the patella is pointing directly anterior. A dose of prophylactic antibiotics with gram-positive coverage is administered in the operating room prior to the skin incision. C-arm fluoroscopy is positioned on the side of the contralateral leg and is used throughout the procedure to ensure ideal positioning of the fixator.
Anesthesia
General anesthesia is typically used to provide analgesia for the surgery. Paralyzing medications are not used as they may mask early signs of nerve irritation from a glancing wire.6
Fibular Osteotomy and peroneal N. release
A transverse incision is made at the level of the fibular neck to identify the peroneal nerve. It was released proximally as well as the first tunnel. Then the fascia between the lateral anterior compartments is released. The intramuscular fascia was divided down to the bone for complete peroneal nerve release. Then separate incision is made between the proximal and middle thirds of the fibula longitudinally. We went between the posterior and lateral compartment muscles. Sub periosteal dissection was done and an oblique osteotomy performed using the saw. Care is taken when performing the sub periosteal dissection as the motor branch to the extensor hallucis longus lies close to the anteromedial border of the fibula. We completed it with an osteotome. We then used the fasciotome to complete both an anterior fasciotomy, lateral fasciotomy, and posterior fasciotomy all from this incision.
Femoral Frame
Two 2/3 rings were selected and applied with the opening of the frame facing posteriorly in the distal frame and medially in the proximal frame. Rotary frame angle of the reference (distal) frame was set as 60º externally rotated. The frame was applied to the leg with 5 or 6-mm hydroxyapatite-coated pins. The ring is held in a position orthogonal to the mechanical axis in the frontal & sagittal views.
Tibial frame
Tibial osteotomy is performed according to the level of the deformity. With use of the fluoroscopic projection, a smooth 1.8-mm wire is advanced across the proximal tibia metaphysis from lateral to medial, perpendicular to the proximal tibia mechanical axis. We prefer to use a 2/3 ring proximally to accommodate posterior leg swelling and allow knee flexion. The ring is held in a position orthogonal to the mechanical axis of the tibia in the frontal and sagittal plane. Then a TSF full ring is applied distally using three 5 or 6-mm half pins in the distal fragment. Struts are attached; typically, medium struts are used with anticlock wise configuration.
Osteotomy
To carry out the osteotomy, the struts are detached from the proximal ring. The osteotomy we use is a percutaneous drill-hole technique. A 1-cm incision is made over the planned site. The incision is carried down through the periosteum. A 5- mm elevator is used to gently raise a portion of the periosteum on either side. The cortex is predrilled in multiple directions along the same plane with a 3.2-mm drill. Lateral fluoroscopy helps to prevent passing the drill or osteotome into the posterior compartment as it traverses the posterior cortex. A 5-mm osteotome is advanced through the cortical bone of the medial and lateral cortices. (Fig.5). When the osteotome is fully seated through the width of the bone and is engaging the posterior cortex, it is twisted producing an audible crack as the posterior cortex fails. The distal ring is gently externally rotated with respect to the proximal ring to ensure that the osteotomy is complete. The bone ends are reduced to their preosteotomy position, relieving stress on the periosteum and decreasing bleeding. The struts are reattached to the rings at their previously measured lengths, stabilizing the osteotomy site in a nondisplaced position. The wound is closed with simple sutures, and the pin sites are dressed with sterile dressings.
Mounting Parameters
Measurement of the four mounting parameters which include A.P, LAT, Axial and Rotatory view offset is taken either in the operating room under C arm control using a sterile ruler or on the postoperative X ray. All deformities were analyzed using total residual mode, correction started 7 days after the surgery, we entered deformity parameters into the TSF web based software computer program and generated an adjustment schedule. The program requires input of deformity, frame, and mounting parameters, and a structure at risk, which determines the rate of correction. The patient is instructed to perform gradual adjustments of the six struts of the TSF once per day.
Postoperative care
In most cases, the patient was discharged between postoperative days 5 and 7. Patients were allowed to either partially or fully weight bear using walking aids such as crutches and/or a walker. Physical therapy was initiated as an inpatient to teach range-of motion exercises, gait training and was also continued in the outpatient setting 2 days a week as range-of-motion exercises initially and then to be followed by stretching and strengthening exercises then pin site care is performed twice per week , patients is encouraged to take a shower with antibacterial soap in the scheduled days for fixator cleaning, then cleaning of the pin sites and the fixator with saline and Betadine coverage of pin sites with a dry sterile Gauze wrap. Follow up visits were scheduled weekly during the first month and then approximately every 2 weeks until correction was achieved.
At the end of the schedule, we determined the limb alignment with physical examination and radiographs. We inspected the patient standing from the front, back, and side views and focused on iliac crest symmetry and leg alignment. On the long standing radiograph, we measured leg lengths, MAD, and joint orientation angles using the same methods used before surgery. When there was residual deformity, we generated and implemented another correction schedule
Frame removal
Our criteria for frame removal are the ability to walk with minimal assistance, when tricortical consolidation was observed on anteroposterior and lateral radiographs, the frame was dynamized for 2 weeks. Fixator was removed and weight bearing was allowed with assistive devices such as a walker and/or crutches
Results
Our study resulted in a mean external fixation time of 5.8 months (range, 2 –11 months). The total time wearing the tibial frame averaged 5.8 months (range, 2-10 months), the total time wearing the femoral frame averaged 6.3 months (range, 2–11 months)
The frame was used dynamically to correct all deformity for a mean time of 4.85 weeks (range, 2–11weeks) whereas the frame was used dynamically to correct Tibia deformity for a mean of 4.3 weeks (range, 2–11 weeks) and dynamically to correct femoral deformity for a mean 6.1 weeks (range, 2–10 weeks).
Our Deformities were reduced from a mean of 25° (range from 10-60°) preoperatively to a mean of 3° (range from 1-7°) at the latest follow up. The mean lengthening was 2.8 cm (range from 1.5-5cm).
Clinical results
The clinical results in our study were asses, at the last follow-up for every case, using Association for the Study and Application of the Method of ILIZAROV (ASAMI) bone and functional scoring system.
Bone Result
Twenty limbs in 16 patients had developed union and consolidation of regenerate in the first instance. Accordingly bone results were excellent in 19 limbs, good in one limb. We have one recurrence of varus deformity in distal femur, patient with metaphyseal dysplasia.
Functional Result
All the 16 patients were able to return to school or activity they were doing prior to treatment, 4 patients had stiffness of the knee that resolved completely with physiotherapy and 2 patients with distal tibia deformities and a foot frame had had stiffness of the ankle. According to ASAMI scoring system the functional results were excellent in 14 patients, good in 2 patients.
Radiographic results
Our radiographic evaluation demonstrated the successful correction of multiplanar distal femoral and tibia deformities in 19 of 20 limbs in 16 patients. The femoral deformities were 4 valgus deformity distal femurs associated with rotational deformity, 3 varus deformity distal femurs, and one shortened limb.
The only unacceptable correction was in a patient with bilateral varus deformity of distal femur and shortening due to metaphyseal dysplasia who had a residual varus deformity on the left side at the time of frame removal on the right side.
With the exclusion to that case, both femoral deformity parameters (mLDFA and PDFA) corrected to within 2º of their normal mean value. Given the normal value for mLDFA of 87º (range, 85º–90°).
The amount of deformity was reduced from a mean of 22.5° (range, 15°–39°) preoperatively to 5° (range, 1–7°) at latest follow up for femoral deformities and with the exclusion to that case, The amount of deformity was reduced to a mean 2° at latest follow up for femoral deformities. The mean amount of femoral lengthening was 3.3 cm (range from 1.5-5cm).
For genu valgum, the mean mLDFA was 75.25° (range, 72–77°) preoperatively and 89° (range, 88– 90°) at latest follow-up. The amount of deformity was reduced from a mean of 18.25° (range, 10–28°) preoperatively to 2° (range, 1–3°) at latest follow up.
For genu varum, the mean mLDFA was 106.6° (range, 102–113°) preoperatively and 94.6° (range, 89–105°) at latest follow up. Given the normal value for mLDFA of 88° (range, 85–90°) , with the exclusion to that case The mean mLDFA was 103.5° (range, 102–105°) preoperatively and 89.5° (range, 89–90°) at latest follow up. Thus, all limbs with genu varum were corrected to within 1°of the normal range. The amount of deformity was reduced from a mean of 28.3° (range, 20–39°) preoperatively to 5° (range, 1–7°) at latest follow up. With the exclusion to that case, the amount of deformity was reduced to a mean 2° at latest follow up for femoral deformities
For the sagittal plane deformity , the aPDFA was 73º preoperatively and 83º at latest follow-up. Given the normal value for aPDFAOf 83º(range, 79º–87º) the amount of deformity was reduced from 5°preoperativey to 0° at latest follow up.
In our study the tibial deformities were 5 varus proximal tibias, 3 external rotation deformities, one valgus ankle, one varus ankle, one recurvatum proximal tibia and one valgus proximal and distal tibia.
The amount of deformity was reduced from a mean of 23.5°(range, 10–25°) preoperatively to 2 (range, 1–5°) at latest follow up for valgus deformities and from a mean of 22.5°(range from 20-25°) preoperatively to 3°(range from 1-5°)at the latest follow up for varus deformities. Recurvatum deformity was reduced from 60°preoperative to 0° at the latest follow up.
Mean rotation deformity was 23.75° (range from 15-40°) preoperatively and is corrected to a mean of 10° postoperatively (range 8-12°)
Tibia deformity parameters (MPTA and LDTA) corrected to within 5º of their normal mean values. Given the normal value of MPTA of 87º (range, 85º–90).The amount of MPTA was reduced from a mean of 95.5º (range, 95-96º) preoperatively to 88.5º (range, 87–90º) at latest follow up in valgus deformity, and from a mean of 68.3º (range, 51–75º) preoperatively to 90.5º(range, 87–95º) at latest follow up in varus deformity.
The amount of (LDTA) was reduced from a mean of 77.5º (range, 75–80º) to 92.5º (range, 90-92º) in the valgus deformity and was reduced from a mean of 105°( range101-113°) to 90°(range86-93°)in the varus deformities. Given the normal value for LDTA of 89º (range, 86º–92º).
The aPPTA was reduced in one case of recurvatum deformity from 141º preoperatively to 83ºpostoperatively. Given the normal value for aPPTA of 83º (range, 77º–84º).
Complications
In our series we had 3 patients with pin tract infection. One responded to oral antibiotics; and two required intravenous antibiotics. Femoral frame resulted in knee stiffness in 4 femurs that resolved completely with physical therapy. Patient with bilateral varus deformity of distal femur and shortening due to metaphyseal dysplasia who had a recurrence of varus deformity on the left side after 18 month of follow up after frame removal, Also same patient had a delayed unions underwent bone grafting, extending the external fixation time at the same side. Her mLDFA was113°preoperatively and 95°at the removal of the TSF and 105°at the latest follow up.
One posterior subluxation of the right knee joint in preoperatively stable knees in a patient with bilateral genu valgus. This case was treated with just aggressive physical therapy (one side) and same patient had residual valgus deformity of 3 deg. on her left femur.
One complication of neuroprexia of the motor branch of the extensor hallucis longus nerve occurred during fibular osteotomy in a patient with proximal varus deformity of the tibia that fully recovered 3 month after surgery.
Another 4 deg. of residual valgus deformity of the tibia after healed congenital tibial psuedoarthosis in one patient, same patient along with another one with distal tibial deformities and foot frame applied has a decrease of the range of motion of the ankle.
One patient with bilateral varus of the proximal tibia had an overcorrection of 5º on the left side.
Discussion
Gradual correction for the management of femoral and tibial deformities by external fixation has become a standard procedure over recent decades. Better understanding of the reaction of bone and soft tissue to gradual distraction has resulted in a reduction of the historically high complication rate and improvement of functional outcome in correction of severe deformities with or without leg length discrepancy.7
The TSF has been in clinical use for more than 10 years. To date, several studies have been published about its clinical application, but only a few addressed limb deformity correction.7
The purposes of this study were 1. to determine the accuracy of TSF in correction of different deformities (i.e., frontal, rotational, and sagittal plane deformities) by evaluating radiological outcome comparing the preoperative and postoperative measurements; 2.To gather the descriptive data on time spent in frame, mean correction time 3.To determine the safety of the use of TSF by reviewing the complications.
There are several limitations to this study due to our lack in the use of TSF as it is not that popular within the Middle East especially the Arab world because of its high price in comparison to Ilizarov external fixator as mentioned in the only international published paper from the whole Arab world and one of the oldest in TSF literature from Egypt.( The cost of the TSF is high enough to limit the frequency that we could use it—about US $4,500 compared to US $500 for an IEF).8
Twenty limbs of 16 patients were included. Even within these limitations, this study describes a series of distal femoral and tibial deformities corrected with a single method. We were able to determine the effectiveness of the TSF and the obstacles encountered.
Our study resulted in a mean external fixation time of 5.8 months (range, 2–11 months). Eidelman et al.9 reported the mean time in the frame as 3.1 months (range, 2–5 months). Sluga et al.10 reported the mean external fixation time as 9.4 months (range, 5.4–12.1 months).
Our radiographic evaluation demonstrated the successful correction of multiplanar distal femoral and tibial deformities in 19 of 20 limbs in 16 patients. The only unacceptable correction was in a patient with bilateral varus deformity of distal femur and shortening due to metaphyseal dysplasia who had a residual varus deformity on the left side at the time of frame removal on the right side. With the exception of that one case, both femoral deformity parameters (mLDFA and PDFA) corrected to within 2º of their normal mean values
The amount of deformity was reduced from a mean of 22.5° (range, 15°–39°) preoperatively to 5° (range, 1–7°) at latest follow up for femoral deformities. With the exclusion to that case, the amount of deformity was reduced to a mean 2° latest follow up for femoral deformities. The mean amount of femoral lengthening was 3.3 cm (range from 1.5-5cm).
For genu valgum, the mean mLDFA was 75.25° (range, 72–77°) preoperatively and 89° (range, 88– 90°) at latest follow-up. The amount of deformity was reduced from a mean of 18.25° (range, 10–28°) preoperatively to 2° (range, 1–3°) at latest follow up.
For genu varum, the mean mLDFA was 106.6° (range, 102–113°) preoperatively and 94.6° (range, 89–105°) at latest follow up. Given the normal value for mLDFA of 88° (range, 85–90°) with the exclusion to that case The mean mLDFA was 103.5° (range, 102–105°) preoperatively and 89.5° (range, 89–90°) at latest follow up. Thus, all limbs with genu varum were corrected to within 1°of the normal range. The amount of deformity was reduced from a mean of 28.3° (range, 20–39°) preoperatively to 5° (range, 1–7°) at latest follow up. With the exclusion to that case, the amount of deformity was reduced to a mean 2° at latest follow up for femoral deformities.
For the sagittal plane deformity, the aPDFA was 74º preoperatively and 83º at latest follow-up. Given the normal value for aPDFAOf 83º (range, 79º– 87º)
Femoral deformities was evaluated by Marangoz et al retrospectively reviewed the clinical and radiographic records of 20 patients (22 limbs), both femoral deformity parameters (mLDFA and PDFA) corrected to within 3ºof their normal mean values. The amount of deformity (absolute difference from the normal mean mLDFA) was reduced from a mean of 15º (range, 4–40º) preoperatively to 2.1º(range, 1–7º) at latest follow-up in genu valgum, and from a mean of 11.9º (range, 3–23º) preoperatively to 1.5º(range, 0–3º) at latest follow-up in genu varum. The amount of procurvatum deformity (absolute difference from the normal PDFA value of 83º) was reduced from a mean of 23º (range, 13–33º) to 0.8º (range, 0–1º).11
Of the five children treated with the TSF by Sluga et al.10, the four with femoral deformities had a mean valgus correction of 9.75º, lateral translation correction of 7.5 mm, and lengthening of 6.9 cm. They reported excellent results for two patients but noted the other two would require further lengthening.
Rozbruch et all retrospectively reviewed 102 patients (122 tibiae) with tibial deformities treated with percutaneous osteotomy and gradual correction with the TSF. The total time wearing the frame averaged 130 days (range, 71–355 days), whereas the frame was used dynamically to correct deformity for 34 days (range, 7–99 days) and results were summarized in the following tables.12
Excellent
Good
Fair Poor |
Union, no infection, deformity<7°,limb length discrepancy<2.5 cm Union + any two of the following: Union +only one of the following: Nonunion / refracture / union + infection + deformity>7° + limb length |
|---|---|
|
Functional Result |
Excellent
Good Fair
Poor Failure |
Active, no limp, minimum stiffness(loss of <15°knee extension/<15°dorsiflexion of ankle),no reflex sympathetic dystrophy, insignificant pain Active with one or two of the following: Limp, stiffness, RSD, significant pain. Active with three or all of the following: Inactive(unemployment or inability to return to daily activities amputation |
Table 1 ASAMI Score
Osteotomy site |
Varus |
valgus |
Apex ant. |
Apex post. |
Internal rotation |
External rotation |
|---|---|---|---|---|---|---|
Proximal tibia |
13(4-46) |
13(4-30) |
11(4-35) |
10(5-20) |
15(10-40) |
14(5-25) |
Distal tibia |
12(5-25) |
17(12-30) |
9(2-22) |
10(4-17) |
5(5) |
18(10-30) |
Table 2 Taylor Spatial Frame deformity parameters for the entire cohort (degrees)
Preoperative deformity |
Preoperative MPTA |
Postoperative MPTA |
|---|---|---|
Preoperative MPTA less than 90 (varus) |
80 (40–89) |
89 (80–97) |
Preoperative MPTA 90 or greater (valgus) |
96 (90–123) |
85 (74–101) |
Table 3 Preoperative versus postoperative MPTA for the proximal group (degrees)
Preoperative deformity |
Preoperative LDTA |
Postoperative LDTA |
|---|---|---|
Preoperative MPTA less than 90 (valgus) |
77 (75–79) |
86 (82–88) |
Preoperative MPTA 90 or greater (varus) |
101 (90–111) |
90 (90–92) |
Table 4 Preoperative versus postoperative LDTA for the distal group (degrees)
|
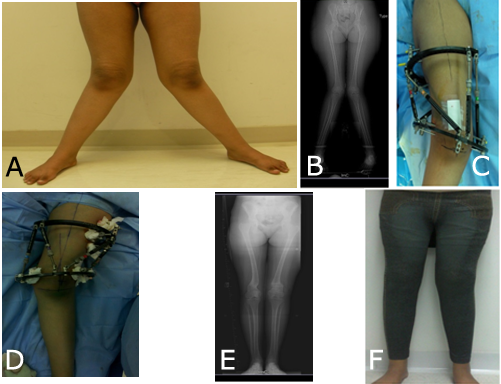
Figure 1 Showing a case of bilateral genu valgum. A, B preoperative photo &X-rayC, D TSF applied. E, F postoperative X-ray&photo. |
Postoperatively, all patients had less than 5º of coronal plane deformity and 15 of 17 patients had less that 5º of sagittal plane deformity. All rotational deformities were corrected.12
In our study the mean we operated upon 12 tibia.The tibial deformities were 5 varus proximal tibias, 3 external rotation deformities, one valgus ankle, one varus ankle, one recurvatum proximal tibia and one valgus proximal tibia.
The total time wearing the tibial frame averaged 5.8 months (range, 2-10 months), whereas the frame was used dynamically to correct deformity for 4.3 weeks (range, 2–11 weeks).
The amount of deformity was reduced from a mean of 23.5°(range, 10–25°) preoperatively to 2 (range, 1–5°) at latest follow up for valgus deformities and from a mean of 22.5°(range from 20-25°) preoperatively to 3°(range from 1-5°)at the latest follow up for varus deformities. Mean rotation deformity was 23.75° (range from 15-40°) preoperatively and is corrected to a satisfactory degree in all cases.
Tibial deformity parameters (MPTA and LDTA) corrected to within 5º of their normal mean values. Given the normal value of MPTA of 87º (range, 85º–90).The amount of MPTA was reduced from a mean of 95.5º (range, 95-96º) preoperatively to 88.5º (range, 87–90º) at latest follow up in valgus deformity, and from a mean of 68.3º (range, 51–75º) preoperatively to 90.5º(range, 87–95º) at latest follow up in varus deformity.
The amount of (LDTA) was reduced from a mean of 77.5º (range, 75–80º) to 92.5º (range, 90-92º) in the valgus deformity and was reduced from a mean of 105°( range101-113°) to 90°(range86-93°)in the varus deformities. Given the normal value for LDTA of 89º (range, 86º–92º).
The aPPTA was reduced in one case of recurvatum deformity from 141º preoperatively to 83ºpostoperatively. Given the normal value for aPPTA of 81º (range, 77º–84º).
Fadel and 8 used the TSF in 22 patients for the correction of lower-limb deformities including lengthening in three patients with congenitally short femurs, and deformity correction and lengthening in one with a posttraumatic femoral fracture. Although the findings from this small subgroup of patients could not be isolated, the overall results were 18 excellent, two good, and two fair.
In our series we had 3 patients with pin tract infection. One responded to oral antibiotics; and two required intravenous antibiotics. Femoral application of an external fixator resulted in knee stiffness in 4 femurs that resolved with physical therapy. One patient with delayed unions underwent bone grafting, extending the external fixation time. One significant complication was posterior subluxation of the knee joint in preoperatively stable knees. This case was treated with just aggressive physical therapy (one patient). The potential risk for posterior subluxation of the knee exists with external fixators, and as we found, including the TSF. Although it is most often associated with the correction of a severe deformity, during a major lengthening, during simultaneous femoral and tibial lengthening, and in inherently unstable knee joints, Jones and Moseley13 reported posterior knee subluxations with as little as 2.5% of distraction. Additionally, subluxations can occur, as happened in one of our cases, in preoperatively stable knees. Close monitoring of the patients through frequent follow-up visits is the only way to avoid this complication
Eidelman et al.9 reviewed their experience on the use of TSF in both tibia and femur. Complications included pin tract infections in two, fracture of the regenerated femur after frame removal in two, femoral fracture after a fall in one, delayed union in one, and residual femoral deformity in a patient with skeletal dysplasia. In our serious we had the same last complication with a patient with bilateral varus deformity of distal femur and shortening due to metaphyseal dysplasia who had a residual varus deformity on the left side after 18 month of follow up after frame removal.
After Eidelman et al.9experienced three fractures, the authors suggested that removing the frame relying on radiographic evidence is inadequate for determining the extent of bone healing, and advocated dynamizing the frame to prevent fractures. One way of dynamizing a Taylor spatial frame is to replace the TSF struts with Ilizarov rods and loosen them to have dynamization. Another option could be either to back out the struts to obtain some compression or take out some wires and/or pins. Another method could be to remove one of the struts, and allow the patient full weight-bearing on the frame. Since this will break the hexagonal construct and make the whole frame unstable, removing one or more struts of the TSF is subject to fractures if the bone is not healed enough. In our series we replaced the TSF struts with Ilizarov rods and loosen them for the cases we saw in need of dynamization and we did not experience any fractures related to early frame removal.
In the study by Sluga et al.10, complications included pin tract infections, temporary knee stiffness, and pin breakage. Complications reported by Fadel and Hosny8,consisted of pin tract infections in all of the patients (12 required antibiotics), adjustment under anesthesia in six, frame loosening in three, early consolidation in three, fracture of the regenerate in two after premature removal of the fixator, and deep vein thrombosis in one. These authors additionally reported the patients had problems following the instructions of the TSF protocol.
In our study we had one complication of neuroprexia of the motor branch of the extensor hallucis longus nerve occurred during fibular osteotomy in a patient with proximal varus deformity of the tibia that fully recovered 3 month after surgery.
We did not experience any frame loosening, early consolidation, pin breaking, adjustments under anesthesia, deep venous thrombosis and our patients which most of them are Arabs didn’t have any problems following the instructions of the TSF protocol.
Conclusion
Based on our results, we believe the TSF allows for the safe, gradual correction of distal femoral and tibial deformities in children and young adults. It is accurate and well-tolerated, with a complication rate that is comparable to the Ilizarov external fixator. And to overcome the problem of the cost of the TSF, we started reusing the frame components after proper cleaning and lubrication of struts and the rings when they are removed from the patient and from our experience we can say that the struts with proper cleaning and storage can be used in 2 or 3 patients without any affection on the accuracy of the correction
References
- www.Orthobullets.com
- Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J. Pediatr. Orthop. 2006; 26:794–798.
- The Apparatus: Components and biomechanical principles of application. In: Transosseous, osteosynthesis. Berlin, Germany. Springer; 1992:63–120.
- Manner HM, Hubel M, Ganger R. Accuracy of complex lower limb deformity correction with external fixation: comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J.Child Orthopedics 1(1):55-61.
- Paley D, editor. Principles of deformity correction. Berlin: Springer-Verlag; 2002.pp. 411–436.
- S. Robert Rozbruch, MD, Austin T. Fragomen, MD, and Svetlana Ilizarov, MD. Correction of tibial deformity with use of the Ilizarov-Taylor spatial Frame. The Journal of Bone& Joint Surgery · JBJS.Org Volume 88-a· Supplement 4 · 2006.
- Rudolf Ganger & Christof Radler& Bernhard Speigner& Franz Grill . Correction of post-traumatic lower limb deformities using the Taylor spatial frame. International Orthopedics (SICOT) (2010) 34:723–730.
- Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int. Orthop. 2005; 29:125–129.
- Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame.JPediatr. Orthop. B. 2006 Nov; 15(6):387-395.
- Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor spatial Frame. J. Pediatric Orthop. B. 2003; 12: 123–128.
- Salih Marangoz, MD. David S. Feldman, MD. Debra A. Sala MS, PT. Joshua E. Hyman, MD. Michael G. Vitale, MD. Femoral deformity correction in children and young adults using Taylor spatial frame. Clin. Orthop. Related Research (2008) 466:3018–3024.
- S.RobertRozbruch, Kira Segal BA, Svetlana Ilizarov, MD, Austin T. Fragomen, MD, Gabriel Ilizarov, MD. Does the Taylor Spatial Frame accurately correct tibial deformities. Clinical orthopedics related research.
- Jones DC, Moseley CF. Subluxation of the knee as a complication of femoral lengthening by the Wagner technique. J. Bone& Joint Surg. Br. 1985; 67:33–35.



