Volume : 1 | Issue : 2
Research
Surgical approach of transmigrated mandibular canine preserving midline of the mandibular symphysis: report of a case
Rodríguez Sáenz Álvaro A,1 Rodríguez Sáenz Diego M,2 Hatem Gammaz Rana,3 Fernández Olarte Humberto4
1Faculty of Dentistry, Universidad El Bosque, Colombia
2Faculty of Medicine, Universidad del Tolima, Colombia
3Faculty of Dentistry, Suez Canal University, Egypt
4Department of Oral and Maxillofacial Surgery, Hospital Simón Bolivar, Colombia
Received: July 04, 2018 | Published: July 25, 2018
Abstract
Transmigration, is an intraosseous displacement of an unerupted tooth in which a movement phenomenon causes it to cross midline by more than half. There are some complications associated with its extraction like, inflammation, mild to moderate pain, and alterations of the contour of the mandibular symphysis. Periosteum and symphysis cortical midline preservation, as well as, grafting with particulate bone mixed with Platelet-enriched fibrin glue and FRP membrane, improve bone regeneration and decrease aesthetic complications associated.In this article, we aim todiscuss a case report of a transmigrated mandibular canine with symphysis cortical midline preservation to decrease aesthetic sequels on the soft tissue.
Keywords: mandibular canine, platelet-rich fibrin (PRF), tissue regeneration
Abbreviations
PRF, platelet-rich fibrin; MSCs, mesenchymal stem cell; hDPSCs, human dental pulp stem cells
Introduction
Transmigration, is an intraosseous displacement of an unerupted tooth in which a movement phenomenon causes it to cross midline by more than 50 %.1 This is an unusual phenomenon with a prevalence up to 0.31% and the etiology of canine transmigration differs from one case to another.2 Several authors have reported genetic predisposition, tumors, abnormal displacement of the dental lamina during the embryonic life, traumatic fracture near the site of mandibular canine eruption, and other local factors.3
Mupparapu et al.1 classified transmigrated mandibular canines, taking into account inclination, relationship with the midline, adjacent teeth and contralateral erupted canine. Type 1: Canine positioned mesioangularlywith the crown portion of the tooth crossing the midline within the jaw bone. Type 2: Horizontal impacted canine next to the lower border of the mandible and below the incisors Type 3: Mesially or distally eruption of the canine according to the opposite canine. Type 4: Impacted horizontal caninebelow of premolars or molars on the contrary side and next to the lower border of the mandible. Type 5: Vertical Canine positioned in the midline (Figure 1).

|
Figure 1 Representation of the unilaterally transmigrated mandibular canines classification according to Mupparapu.1 |
Impaction of canines is more common in the maxilla with an incidence ranging from 0.92% to 5.1% and transmigration is more common in the mandible with an incidence ranging from 0.1% to 0.31, mostly affecting the lower canines than the uppers and usually existing unilaterally more commonly than bilaterally.3,4 Presently, there are several treatment options available to address transmigrated canines, including radiographic observation, autogenous transplantation, orthodontic treatment and tooth extraction when there is inadequate space to realign the tooth.5 There have been incidences of complications associated with the extraction of impacted teeth like trismus, inflammation, mild to moderate pain, hematoma and bony defects.6 Different studies have reported that some patients who have been operated on the symphysis, suffered changes in their facial contour and aesthetic changes in the symphysis zone.7
Case report
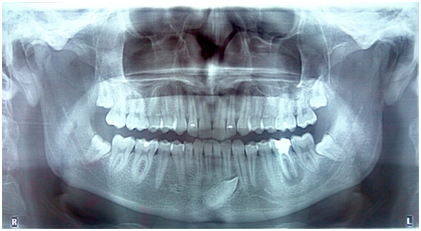
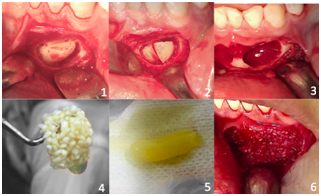
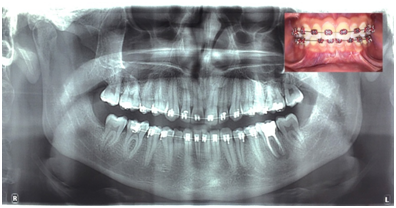
A 22years old symptomatic male patient, was referred to our dental clinic presenting a transmigrated mandibular canine. During oral examination, crowded mandibular incisors, as well as a missing right permanent canine (27) and an over-retainedright deciduous canine (R), were observed. Panoramic examination revealed a mesio-angular transmigrated mandibular caninetype I (Figure 2). Due to the crowded incisors and insufficient space in the arch, surgical extraction with local anesthesia was performed. Under informed consent of the patient and strict aseptic conditions, a traditional bilateral inferior alveolar nerve block was administered to anesthetize the mandibular nerve 1.2mL of Roxicaina® (2% Lidocaine with 1:80.000epinephrine). Semilunar incision and dissection of the flap was performed. Pericoronalostectomy and cross-sectioning of the crown was done. An additional surgical window was performed to preserve midline and tooth extraction was carried out. The socket was filled with particulate bone mixed with Platelet-enriched fibrin glue and a PRF membrane was placed on the grafting (Figure 3). Finally, healing by first intention was facilitated by continuous suture. After 8days, control was done and the patient reported mild pain, swelling, trismus and hematoma in the mental region. Orthopantomographywas taken 6months after procedure (Figure 4).
Discussion
Mandibular canine transmigration is a very uncommon anomaly which reportedly occurs in about 5% of cases.8 It can be associated with several postoperative complications like pain, swelling, trismus and hematoma similar to that of a common impacted tooth extraction.9 Likewise, several authors have reported that surgical approaches performed in the chin area can develop bone defects and a negative correlation in the thickness of the chin’ssoft tissue relatedto the center of the defect.10 According to Verdugo et al. in their clinical study, they revealed that bone defects<0.5cc showed an 81% of bone fill during a period of healing of 34.2months, whereas those>0.5cc with a period of 7.2months showed a repair of 63.8% (P<0.05) and this can be influenced by many factors like age, as well as periosteum and symphysis cortical midline preservation of the chin.11 However, full repair of the sites did not occur.
Different approaches of tissue regeneration have been used, in which an ideal bone graft should allow for new bone formation, including osteoconduction, osteoinduction and osteogenesis. Autogenous bone graft has those properties; however, it is indispensable to perform another surgical procedure, and it can increase infection risk, cost and time of the procedure.12 The improvement of common postoperative complications, osseous defects and commitment of mandibular symphysis contour with platelet-enriched fibrin glue and platelet rich fibrin (PRF) has been seen as an excellent scaffold for tissue engineering due to the initial stability, biocompatibility, biodegradability and constant release of growth factors of the PRF, which allows mesenchymal stem cell (MSCs) migration, mineralized differentiation and faster angiogenesis.13 Likewise, according to Kökdere et al.14 combination of particulate bone graft with PRF promotes a greater mean area of newly formed bone compared with the PRF alone.14 To have better outcomes in procedures of this nature, one should perform sulcular incisions, periosteum and symphysis cortical midline preservation and grafting with bone substitutes and PRF. This approach can be improved with the incorporation of the human dental pulp stem cells (hDPSCs) whose osteogenic potential is the highest in our body.
Acknowledgements
Michelle Meyer who provided valuable assistance.
Disclosures
Conflict of interest: The authors report no conflicts of interest related to this study.
Formatting of funding sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical disclosures
- Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
- Confidentiality of data. The authors declare that no patient data appear in this article.
- Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or sub- jects mentioned in the article. The corresponding author is in possession of this document.
Reference
- Mupparapu M. Patterns of intra-osseous transmigration and ectopic eruption of mandibular canines: review of literature and report of nine additional cases. Dentomaxillofac Radiol.. 2002;31(6):355–360.
- Aktan AM, Kara S, Akgünlü F, et al. The incidence of canine transmigration and tooth impactation in a Turkish subpopulation. Eur J Orthod. 2010;32(5):575–581.
- Aktan AM, Kara S, Akgunlu F, et al. Unusual cases of the transmigrated mandibular canines: report of 4 cases. Eur J Dent. 2008;2(2):122–126.
- Kumar S, Jayaswal P, Pentapati KC, et al. Investigation of the transmigrated canine in an orthodontic patient population. J Orthod. 2012;39(2):89–94.
- Kılıç N, Oktay H. Orthodontic intervention to impacted and transposed lower canines. Case Rep Dent. 2017;2017:4105713.
- Manne R, Gandikota C, Juvvadi SR, et al. Impacted canines: Etiology, diagnosis, and orthodontic management. J Pharm Bioallied Sci. 2012;4(2):234–S238.
- Andersson L. Patient self-evaluation of intra-oral bone graft- ing treatment to the maxillary frontal region. Dent Traumatol. 2008;24(2):164-169.
- Torres-Lagares D, Flores-Ruiz R, Infante-Cossío P, et al. Transmigration of impacted lower canine. Case report and review of literature. Med Oral Patol Oral Cir Bucal. 2006;11(2):E171–174.
- Juodzbalys G, Daugela P. Mandibular third molar impaction: review of literature and a proposal of a classification. J Oral Maxillofac Res. 2013;4(2):e1.
- Dik EA, de Ruiter AP, van der Bilt A, et al. Effect on the contour of bone and soft tissue one year after harvesting chin bone for alveolar cleft repair. Int J Oral Maxillofac Surg. 2010;39(10):962–967.
- Verdugo F, Simonian K, D'Addona A, et al. Human bone repair after mandibular symphysis block harvesting: a clinical and tomographic study. J Periodontol. 2010;81(5):702–709.
- St John TA, Vaccaro AR, Sah AP, et al. Physical and monetary costs associated with autogenous bone graft harvesting. Am J Orthop. 2003;32(1):18–23.
- Arunachalam M, Pulikkotil SJ, Sonia N. Platelet rich fibrin in periodontal regeneration. Open Dent J. 2016;10:174–181.
- Kökdere NN, Baykul T, Findik Y. The use of platelet-rich fibrin (PRF) and PRF-mixed particulated autogenous bone graft in the treatment of bone defects: An experimental and histomorphometrical study. Dent Res J (Isfahan). 2015;12(5):418–424.