Volume : 2 | Issue : 1
Research
Health Equity in Nursing: A Concept Analysis
Joel C Estacio1,2
1Faculty, Don Mariano Marcos Memorial State University - College of Community Health and Allied Medical Sciences, Agoo, La Union, Philippines
2Doctor of Philosophy in Nursing Candidate, Saint Louis University, Baguio City, Philippines
Received: October 29, 2018 | Published: January 01, 2019
Abstract
Rationale of the Study: The concept of primary health care has ignited efforts of health leaders to improve the health status of people worldwide. This impelled attempts to reduce inequities through policy changes and interagency collaborative participations. With nurses at the center of the healthcare delivery, they could contribute much to potentiate attainment of equity in health. However, little is known regarding the realization of the concept of health equity from the leaders in healthcare down to the healthcare workers.
Research objectives/Problem statement: This concept analysis provides a thorough review of the concept of health equity in nursing and relatedness to healthcare and health practices.
Methods: A concept analysis method described by Walker and Avant1 was used to clarify the meaning of health equity in Nursing. The concept’s attributes were determined through extensive literature search. Model, borderline, and contrary cases were constructed. Analysis was further done by identifying the antecedents, consequences, and empirical referents of health equity.
Results and Conclusions: Health Equity is attributed to adequate and appropriate distribution of health services which is closely linked to an opportunity to gain access to health services that is not affected by socioeconomic status or other factors. Establishment of relevant policies and effective promoting actions of health and non-health agencies are indispensable to realize health equity. Generally, it is believed that if there is health equity, there will be improvement of the heath status of people. It will yield greatest contributions to maintaining and preserving the rights of people in terms of their health and their right to be not deprived of services from vast network of health systems. Presence of which prevents disadvantaged groups to have greater disadvantage. The concept continues to be a major concern particularly in developing countries where socially disadvantaged population groups are at its highest. Implementation of universal healthcare may continue to be a challenge among health and non-health related organizations. Clearly, more intensive efforts are needed at various levels of policy development and implementation.
Keywords: health equity, concept analysis, social justice, nursing
Introduction
The concept of primary health care has ignited efforts of health leaders that impelled attempts to reduce inequities in health through policy changes and interagency collaborative participations. With nurses at the center of the healthcare delivery, they are envisioned to contribute much to potentiate attainment of equity in health. However, little is known regarding how the concept of health equity as propelled by the healthcare leaders is realized by the healthcare workers particularly nurses.
Since the creation of primary health care, much focus has been made to improve public health through the efforts contributed by the health workforce. During the past decades, the concept of primary health care has generated significant influence particularly among the health workers in many less-developed countries.2,3 This is in response to the inevitable trends in health and health problems across different countries whose objective is to improve health in the community level.
The World Health Organization (WHO) has developed plans and strategies that aim to focus on the Social Determinants of Health to attain what is called equality in health.4 This ignited efforts of health leaders to improve health status worldwide by reducing health inequities within and between countries through policy changes and interagency collaborative participations. 5,6
This concept analysis provides an effort to yield thorough understanding of the concept of health equity and how it relates to healthcare and health practices. Through the concept analysis method described by Walker and Avant1 this paper expounds the meaning of health equity and examines its attributes and characteristics. The results assist to understand the essence of the concept especially for the health workers and help guide theoretical and practical applications in the healthcare practice.
Background
Inequities in health across nations raised concerns on quality of healthcare and justice. Various health organizations have attempted to define health equity. According to the US Department of Health and Human Services, Health equity is “attainment of the highest level of health for all people”.7 They also added that attaining health equity necessitates the need to value everyone equally. This contends that each should be given equal value and equal chance to avoid possible inequalities and injustices.
The US Center for Disease Control and Prevention stated that health equity is achieved when every person has the opportunity to "attain his or her full health potential" and no one is "disadvantaged from achieving this potential because of social position or other socially determined circumstances".8 According to the WHO, Health Equity is the “absence of unfair and avoidable or remediable differences in health interventions and outcomes among groups of people”.
In 2003, Braveman and Gruskin9 defined health equity to guide operationalization and measurement. They defined equity as the “absence of systematic disparities in health (or in the major social determinants of health) between groups with different levels of underlying social advantage/disadvantage – that is wealth, power, or prestige”.
There has also been a wide debate in an attempt to mark the line between health equity, and health inequality not only as to how they are understood but also in terms of how they can be measured.10 In Europe, health inequalities refer to the differences in health between those who live in “better or worse socioeconomic conditions”. Furthermore, Braveman and Gruskin9 emphasized in their review the difference between equity and equality. Equity turns out to be more appropriate when describing unfair distribution of health resources or health services. It is a term that is used to denote unfair or unjust inequality. Inequality can be seen in many societal groups, between and within population groups. This can merely be measured using standard health statistics. Inequity, on the other hand, possess the ethical and moral dimensions of health status and service utilization and access between and within population groups. Equity can be examined through comparison of health status and access in context of what is happening with the rest of the society.11
Much has been made to give definition of the term equity and its application to health and healthcare. A similar characteristic in terms of the exhaustive definition of the term and its use takes along with it the fact that in order for population or groups to have equity in health, there should be fair distribution of health and health services. Other definitions also associate the term with ethical and moral standards wherein it is more ethical to have more distribution of health and for health services to be more readily provided to those who need it more.
Equity in health is also associated with the right of people. Health is said to be a fundamental human right. This is true in all nations. Therefore, every person is as equally entitled to one and if deprived, they are entitled to access services which will bring them to a state of health and wellness.
On the other hand, efforts have been made to develop strategies of creating assessment or evaluation tools to identify inequalities or inequities across several population groups.12 Studies have also been done to determine indicators of health equity in some areas.13,14 These studies help contribute to the attainment of the vision and goals of international health organizations in terms of attainment of equity in health within and between countries.
In order to know beforehand that there is health equity, it must be decided as to how assessment and monitoring of the health status and health service delivery are made in a specific population group. Several organizations, particularly the world health organization, prioritize health and its determinants in establishing a baseline data in terms of attaining health status among various countries.12,14
Walker and Avant’s1 eight steps of concept analysis brings clearer view of the broad concept of health equity as fulfilled by the health workers who are in close contact with their clients. Nurses, who are primarily working with clients in the attainment of health are envisioned to benefit in this concept analysis as they may be provided with scientific and practical use of the concept that will augment quality and just healthcare.
Defining attributes
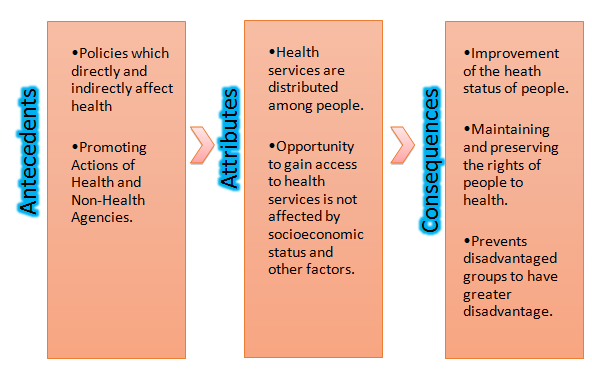
Health equity is seen initially as the state whereby health services are distributed among people. Also, the concept is attributed to an opportunity to gain access to health services between people or population groups that is not affected by socioeconomic status and other factors.
Antecedents
A growing attention on health equity especially among the health leaders and legislators. Public health and health equity has become a global health priority. According to the WHO Director-General Margaret Chan, “Health inequity really is a matter of life and death”.15 This caused attempts among leaders to focus their health and health-related concerns on addressing the issue of inequity in health.
Health equity would not happen without the policies being made by policy makers. Policies greatly affect health and heath status of various people either directly or indirectly. Policies set in place either addressing health or not, could cascade and eventually affect health and equity in health among individuals, families and population groups.6,16
In addition to the policies being made by the policymakers, the promoting actions of health and non-health agencies in the international, national and local levels facilitate the occurrence of health equity. Internationally, the World Health Organization participates in the formulation and implementation of strategies to promote equity in health across different countries.17 Since health equity is being addressed on worldwide scale, the promoting actions are expected to be cascaded from international organizations to local levels, targeting each clientele with consideration and in support of their socio-cultural and political backgrounds.
It has been believed that inequalities in health are shaped by many attributing factors like socioeconomic status, position in labor market, educational status, income, gender, ethnicity, age, place of residence and disability.18 These factors are only contributory to the occurrence of inequities and inequalities. Absence of these factors may not necessarily result to health equity. It was found that many of these factors are under-researched. Although it is said that many groups of population respond differently to health leaders’ efforts and health programs. Such differences that exist may be due to factors identified or other community-level variations..19
Consequences
There are many possible consequences of health equity. Generally, it is believed that if there is equity in health, there will be improvement of the heath status of people. Health equity will yield greatest contributions to maintaining and preserving the rights of people to health and their right to be not deprived of services from vast network of health systems. Presence of which prevents disadvantaged groups to have greater disadvantage.
Empirical Referents
It is extensively recognized that health equity is addressed in major health goals set by global health leaders. Today, several tools have been made to measure health equity. These tools help health organizations to assess and monitor inequities in countries. In addition, these tools contribute to the attainment of health equity across nations by evaluating strategies through outcome measures that relate to health equity.
One of the latest developments in terms of measuring health equity is the Health Equity Assessment Tool. This helps explore and compare data to determine possible inequalities in each data. This tool is software and it was claimed to be user-friendly, interactive and fully flexible format.12
Demographic surveys are also used especially in determining social determinants that predispose the least advantaged to suffer health inequities. In the Philippines, the Department of Social Welfare and Development uses the National Household Targeting System Tool to determine households which are disadvantaged during survey. The result of these household surveys are being collected and consolidated by the Republic of the Philippines’ Department of Health. Data are analyzed and presented. Although these tools do not provide exact measure of health equity, they help contribute to understanding the concept through identifying the least advantaged population groups.20
Case Studies
The cases presented below depict Model cases, Borderline cases, and Contrary Cases to provide further description and understanding of the concept.
Model Case and Analysis
Abigail is a 39-year-old resident of a community in La Union. She is a mother of four children aged 17, 14, 10 and 7 years. She is married to Francis, 45 years old tricycle driver. Their income for a day is about 400 – 500 pesos which is just enough for their basic expenses.
When she got pregnant for her fifth child, she went to the nearest health center located 10 minutes away from their residence on a tricycle. The Rural Health Midwife recognized her upon arrival. The midwife immediately attended to Abigail and provided her with a comfortable place in the waiting area while the midwife got her records. The midwife ensured proper attendance to Abigail in this pregnancy and counseled her regarding her birth plan. Since this is high risk pregnancy, the midwife recommended several accessible hospitals where Abigail could give birth. The midwife reiterated the privileges that Abigail has since Abigail is an indigent member of Philhealth (Philippine Health Insurance Corporation) – the National Health Insurance Corporation in the Philippines. The midwife further explained that even though Abigail is advised to have her birth in a hospital facility, she could still continue to have her prenatal care in the health center since this is more convenient and accessible.
Abigail continued to have a healthy pregnancy and gave birth through normal spontaneous delivery in a district hospital where she was attended to by an obstetrician, a pediatrician, a nurse and a midwife free of charge. During the postpartum care, Abigail was regularly attended to by the rural health midwife. Home visits were subsequently conducted by trained “barangay” health workers. Despite Abigail’s struggles in their household expenses, she was managed to have safe and normal pregnancy and delivery through competent health professionals, proper collaboration and strong intra-sectoral linkages.
The model case presented fully demonstrates all the attributes of health equity. The case presented the availability of a functional health facility in a geographically accessible location to the case participant. In addition, health services were also readily available to the participant throughout pregnancy. Although the services were provided by several health professionals, the case participant received the necessary care she needed from pregnancy to postpartum period. The follow-up care given by the midwife and the “barangay” health workers provided very significant contributions to the successful recovery of the participant throughout the process. Also, the model case participant was given an opportunity to access the health services due to the provision of adequate counseling and referral of the rural health midwife. The intra-sectoral linkage between the rural health midwife and the district hospital was evident in the proper referral of the high risk patient. In the district hospital, the participant was taken cared by specialized healthcare professionals. In the Philippines, universal health care is aimed to attain through efforts and collaboration with the National Health Insurance System. Anchored on the belief that health is a fundamental human right, the Philhealth furnished a scheme of providing membership for the indigents of society – those who are unable to pay for their monthly contributions. With this, they are able to enjoy health services without being able to think about the possible out-of-pocket expenses. The model case participant was able to receive health services through her indigent membership. These attributes made the participant to receive the necessary health care services she needed.
Borderline Case and Analysis
Shiela is a 19 years old single mother who currently resides with her parents. Together with her two-year-old son, she stays at home throughout the day to take care of the household chores while her parents are trying to make a living in the market. One day, she noticed her son to have high fever. She has been giving her son herbal preparations for cough during the past two days and thought the remedy would make her son feel better, but now she noticed her son to be getting worse. She continued to give the herbal preparation, still hoping it would help her child to get better through the day. She wanted to take her son to the health center but she would have to travel 15 minutes on foot and wait for the “jeepney” to take them to the nearest health center for the succeeding 40 minutes. In addition, she would need money to pay the transport and possible expenses during the health visit and to purchase medications for her child. What she did was just to wait for her parents to arrive in the afternoon. Her parents saw the condition of the poor child and noticed it would need to be taken to a doctor for treatment or else they would regret it. The child was taken to the nearest health center in the middle of the night but then there was no doctor and adequate health facilities that could help the child with his current condition. The child was referred to the nearest district hospital and there the child was admitted and managed as a case of Severe Pneumonia. With meager financial capacity, the child’s bill was waived and was taken cared by the hospital specialists. It took them seven hospital days. The child was discharged and recovery was continued at home. However, Shiela’s parents took home with them thousands of pesos of credits because of the non-hospital expenses like food and transportation during the child’s hospital stay. Although the hospital bill was covered by the national insurance, they are still faced with the challenge of being able to recover financially.
This borderline case represents attainment of most attributes of health equity. Healthcare services were not fully distributed and not readily accessible in their place. This raises attention in terms of extent of accessibility of health facilities and health services. It affected the health seeking behavior demonstrated by Shiela. Despite the presence of the health facility, Shiela preferred to resort to herbal remedies. Also, opportunity to access the nearest health center was poorly met due to challenges in transportation. Health policies were in place. The family benefited from the no billing scheme of the health insurance. However, clearly, the family was already disadvantaged due to the geographic location of their residence. This further complicated the problem when they were referred to the nearest hospital because of lack of a medical doctor in the health center.
Contrary Case and Analysis
Romy is a 32-year-old family man who lives in a seaside community. He resides with his wife, three children and her 58-year-old mother. He is the only member of the household who earns for his family. He has been working as a branch manager of a fast food chain for five years. His mother was diagnosed with Type II Diabetes Mellitus 19 years ago. Her condition was carefully managed until last year when she was found to have developed kidney failure and was advised to undergo hemodialysis. She underwent the treatment at about two sessions weekly. Because she was enrolled in the Philhealth as a dependent of Romy, she used the benefits provided by the insurance during treatment sessions. However, Romy had difficulties in sustaining adherence of his mother to undergo hemodialysis sessions due to other expenses not covered by the health insurance such as transportation, food, and other out-of-pocket hospital bills. Because of this, they inevitably missed most treatment sessions which resulted to the condition of his mother to become worse.
One day, Romy’s mother needed to stay for longer in the hospital because of extreme body weakness and anemia. Romy was forced to sell most of their appliances to sustain his mother’s healthcare needs. In addition, his mother needed some blood transfusions to cope with her alarming hemoglobin result. Blood was oftentimes unavailable in the hospital which is why Romy went to different blood banks and neighboring hospital facilities in search for available blood for his mother’s transfusion therapy. Time passed by and his mother sought more health services to get through with her worsening condition and needed to stay in the hospital most of the time. Romy was forced to stay in the hospital in most occasions because his wife needed to be at home to accompany their children. This made Romy acquire more absences in his work. His burden became more pronounced as his mothers’ condition grew worse due to lack of adherence to the treatment regimen brought by constraints in time, work, and money.
Romy and his mothers’ burden and suffering were pushed beyond their limits when his mother was again admitted to the hospital because of severe anemia, extreme body weakness and dizziness. She stayed in the hospital while Romy was in search for financial support, blood and blood donors for her mother’ blood transfusion. Romy was told by the doctor that if he could not find a blood donor or blood from other blood banks, his mother may not make it. It was also emphasized that the best thing that the hospital can do for now is to wait for Romy to bring donors or blood from other blood banks. He contacted his relatives and friends who could help them by asking for more money to lend, and possibly for another blood donation. As he expected, everyone already gave most of their savings. With barely enough money to cover transportation, Romy hopped from one blood bank to another. Because compatible blood was unavailable in all blood banks, his mother did not receive blood transfusion. Her condition got worse. Romy and his family were hopeful but his mother did not make it.
This is an illustration of a contrary case since all of the attributes were absent. A demonstration of lack of equity in health among those who do not belong to the poorest of the poor but in the middle class was exemplified in this case. Romy was initially disadvantaged because of inadequate financial capabilities. He sustains all the household expenses and his financial capability was challenged to its limits when his mother was diagnosed to have End Stage Renal Disease and needed Hemodialysis. It’s a good thing that Romy’s membership in the Health Insurance covered his mother. They were able to feel the benefit of the help given by the Health Insurance company. However, not everything was covered and Romystill had much out-of-pocket expenses. This further made Romy decide to look for other alternative sources to pay for the expenses. This condition made his mother suffer even more because they had no choice but to skip sessions because of financial inadequacy. Romy also struggled in search for available blood for transfusion. In the case, the hospital where Romy’s mother was confined, did not have any available blood for transfusion. All the health workers did was just to wait for Romy to find the needed blood for his mother’s transfusion.
Conclusions
Figure 1 above shows how the concept of health equity can be further understood by defining its antecedents, attributes, and consequences.
In this concept analysis, it was found that health equity is a general term that describes the general health status of the public. The concept is still a major concern particularly in developing countries where socially disadvantaged population groups are at its highest. Implementation of universal healthcare may continue to be a challenge among health and non-health related organizations. Clearly, more intensive efforts are needed at various levels of policy development and implementation. Involvement of the community and special population groups may provide useful contributions to strengthen health equity in nursing. Groups like those which aim to raise awareness of the public in terms of inequity and health rights may provide great contributions to strengthen equity and fairness of opportunities. In areas where health service delivery is provided mostly by “barangay” health workers, relevant skills trainings may provide indispensable competencies to available manpower who render health services. A strong focus on adequacy and sufficiency of health facilities and resources, manpower, and accessibility of health facilities are important factors that policy makers and health leaders must focus on.
References
- https://www.pearson.com/us/higher-education/program/Walker-Strategies-for-Theory-Construction-in-Nursing-5th-Edition/PGM146725.html
- Hotchkiss DR, Banteyerga H, Tharaney M. Job satisfaction and motivation among public sector health workers: evidence from Ethiopia. Hum Resour Health. 2015;13(1):83.
- Cueto M. The origins of primary health care and selective primary health care. Am J Public Health. 2004;94(11):1864–1874.
- WHO | About the Health Equity Monitor. http://www.who.int/gho/health_equity/about/en/. Accessed November 15, 2018.
- Lathrop B. Nursing leadership in addressing the social determinants of health. Policy Polit Nurs Pract. 2013;14(1):41–47.
- Gama e Colombo D. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Rev Direito Sanitário. 2010;10(3):253. doi:10.11606/issn.2316-9044.v10i3p253–266
- National Stakeholder Strategy for Achieving Health Equity. :233.
- CDC - Attaining Health Equity - Healthy Communities Program. https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/overview/healthequity.htm. Accessed November 15, 2018.
- Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health. 2003;57(4):254–258.
- Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194.
- Whitehead M. The concepts and principles of equity and health. Health Promot Int. 1991;6(3):217–228.
- Hosseinpoor AR, Nambiar D, Schlotheuber A, Reidpath D, Ross Z. Health Equity Assessment Toolkit (HEAT): software for exploring and comparing health inequalities in countries. BMC Med Res Methodol. 2016;16(1):141.
- Cookson RA, Asaria M, Ali S, et al. Health Equity Indicators for the English NHS: a longitudinal whole-population study at the small-area level. Health Serv Deliv Res. 2016.
- Hosseinpoor AR, Bergen N, Koller T, et al. Equity-oriented monitoring in the context of universal health coverage. PLoS Med. 2014;11(9):e1001727.
- WHO | Inequities are killing people on grand scale, reports WHO’s Commission. WHO. http://www.who.int/mediacentre/news/releases/2008/pr29/en/. Accessed November 15, 2018.
- Finnegan SC, Cheng N, Bazemore AW, Rankin JL, Petterson SM. The changing landscape of primary care HPSAs and the influence on practice location. Am Fam Physician. 2014;89(9):Online.
- Hosseinpoor AR, Bergen N, Schlotheuber A. Promoting health equity: WHO health inequality monitoring at global and national levels. Glob Health Action. 2015;8(1):29034.
- WHO | Social determinants of health. WHO. http://www.who.int/social_determinants/en/. Accessed November 15, 2018.
- Molla AA, Chi C, Mondaca ALN. Predictors of high out-of-pocket healthcare expenditure: an analysis using Bangladesh household income and expenditure survey, 2010. BMC Health Serv Res. 2017;17(1):94.
- PSA PSA. Philippines National Demographic and Health Survey 2013. 2014.