Volume : 1 | Issue : 1
Commentary
Vaccine –the blessing to human kind
Dr. Hemant Patel
Family Physician and Vaccinologist, India
Received: June 19, 2018 | Published: August 03, 2018
Abstract
Immunization is a process whereby a person is made immune or resistant to infectious disease, typically by the administration of a vaccine. Vaccines stimulate the body's own immune system to protect the person against subsequent infection or disease. The World Health Organization organizes the World Immunization Week every year to highlight the collective action needed to ensure that every person is protected from vaccine preventable disease with different themes. This year the World Immunization Week was held from 24-30 April 2018 with the theme "Protected Together". The main aim of this theme is to encourage people to go further in their efforts to increase the Immunization coverage. It has been estimated that 22.6 million infants worldwide are still missing out on basic vaccines, mostly in the developing countries, which can be devastating at times due to malnutrition, poverty and lack of education in the developing countries. Thus, Immunization is essential for each and every individual to protect themselves as well as others from many life threatening diseases. One famous line as said by William Foege-" Vaccines are the tugboats of preventive health".
Introduction
Adults are 60% of our population and the most economically productive age group. However, they often neglect their health while taking care of others. Waning immunity from childhood vaccines, change in target age groups for many Vaccine Preventable Diseases (VPDs), extensive travel, stressful lifestyles and neglect of prevention has led to the increasing burden of VPDs among adults. Gone are the days when vaccines were only for kids. In today's fast paced world, where there is little time to fall ill, vaccinations are becoming imperative for adolescents and adults too. India has a large burden of these diseases and there are many roadblocks that hinder the path of tackling them. This commentary tries to throw light on this burden of diseases and various strategies that can be adapted to upscale adult vaccination in India.
Vaccine Preventable Diseases (VPDs) and Vaccination
There have been major epidemiological changes in the prevalence, affected age groups and susceptibility of infectious diseases. Many diseases once known to affect only children are now seen among adults as well. One such example was seen in former Soviet Union where a massive diphtheria outbreak caused more than 1,57,000 cases and 5000 deaths. Surprisingly, majority of cases occurred in persons >15years old, and very high incidence and death rates was seen among adults from 40 to 49years old.1 A news report recently suggested that more than 95% deaths due to VPDs in India occur in adults.2 Moreover, the morbidity and disability caused by VPDs in a country like India is also huge.3 Apart from the diseases that can be easily prevented through vaccines, there have been emergence and re-emergence of infectious diseases that has further pressurized our already overburdened health system. To name a few, HIV, malaria, multi-drug resistant Tuberculosis and drug resistant Sexually Transmitted Diseases (STDs) are posing a new challenge. In such a situation, more emphasis should be laid on tackling the VPDs that can easily be prevented through vaccination. Vaccination is the most cost effective and powerful weapon of prevention. Vaccination is one of medicine’s greatest accomplishments, reducing and in some cases eradicating once life-threatening diseases such as smallpox and polio.4 Gone are the days when vaccines were only for kids. In today’s fast paced world, where there is little time to fall ill, vaccinations are becoming imperative for adolescents and adults too. Centre for Disease Control (CDC) states “Traditionally, vaccines have been associated with protecting young children, but far too many adults become ill, are disabled, and die each year from diseases that could easily have been prevented by vaccines”.5 Adults are 60% of our population and the most economically productive age group. They often neglect their health while taking care of others. The immunity that children acquire because of vaccination wanes off as they turn into adults making them susceptible to diseases once again. If they acquire the diseases they not only lose some days of productive work but can also infect their little ones. Western world is aware and proactive.
A news report recently suggested that more than 95% deaths due to VPDs in India occur in adults. Moreover, the morbidity and disability caused by VPDs in a country like India is also huge. Apart from the diseases that can be easily prevented through vaccines, there have been emergence and re-emergence of infectious diseases that has further pressurized our already over-burdened health system. To name a few, HIV, malaria, multi-drug resistant Tuberculosis and drug resistant Sexually Transmitted Diseases (STDs) are posing a new challenge. In such a situation, more emphasis should be laid on tackling the VPDs that can easily be prevented through vaccination.
Vaccination is the most cost effective and powerful weapon of prevention. Vaccination is one of medicine’s greatest accomplishments, reducing and in some cases eradicating once life-threatening diseases such as smallpox and polio Gone are the days when vaccines were only for kids. In today’s fast paced world, where there is little time to fall ill, vaccinations are becoming imperative for adolescents and adults too. Center for Disease Control (CDC) states “Traditionally, vaccines have been associated with protecting young children, but far too many adults become ill, are disabled, and die each year from diseases that could easily have been prevented by vaccine. “Adults are 60% of our population and the most economically productive age group. They often neglect their health while taking care of others. The immunity that children acquire because of vaccination wanes off as they turn into adults making them susceptible to diseases once again. If they acquire the diseases they not only lose some days of productive work but can also infect their little ones.
Adult vaccination has many advantages like:
Reduced burden of diseases in the most productive group, Reduced incidence and prevalence of the disease in the population owing to the herd immunity that adult vaccination will Provide Vulnerable groups will have better protection if people around are vaccinated-like infants, people with chronic diseases, pregnant females and elderly people. However, despite of adult vaccination being such a cost-effective strategy, there is no data on adult immunization coverage in India neither are there any recommendations in place and it is assumed that adult immunization is 15-20years behind as far as large-scale acceptance is concerned. There is no focus on adult immunization. Burden of VPDs in India & Vaccinations Available There are various diseases that cripple India’s health system and VPDs are amongst them. India is a developing nation and deaths due to infectious diseases still surpass that due to non-communicable diseases. There is a lack of systematic epidemiological data denning the exact burden of various diseases. However, some sporadic and local data is available that has been summarized below.
Rubella:
Rubella Congenital Rubella syndrome (CRS) is a big public health problem of India. It has been observed that around 40-45% of women in the childbearing age are susceptible to Rubella and over 2lakh babies are born with birth defects because of Rubella infection during pregnancy in the Indian sub-continent.6 CRS ac-counts for 10-15% of paediatric cataract. 10-50% of children with congenital anomalies have laboratory evidence of CRS. According to the Advisory Committee on Immunization Practices (ACIP), all females of childbearing age group should receive 2 shots of MMR vaccine if they are susceptible, at least 3 months before pregnancy. Susceptibility can be ensured by absence of immunization, absence of disease in the past and serological testing. However, serological testing is a costly procedure and requires two visits to the health-care facility-one visit for testing and second for immunization thus immunization should be advised whenever immunity against Rubella is in doubt.
Cervical Cancer:
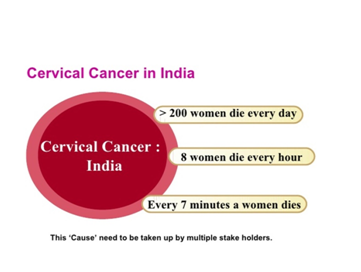
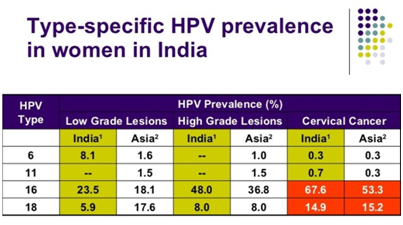
Around 1, 32, 000 women in India each year are detected with cervical cancer and 74,000 of them die.7 The cancer is the second most common cancer in India and has a high mortality (50%), mainly due to lack of awareness and no systematic screening infrastructure in place. The factors leading to high prevalence of cervical cancer in India are many. For e.g., genital hygiene standards are quite low. Of the 355 million menstruating women in India, only 12% use sanitary napkins. Thus, in the present scenario, the best defense we have against cervical cancer is prevention through vaccination. Human Papilloma Virus (HPV) vaccines are two vaccines that have been developed against strain 16 and 18 of HPV that causes most of the cases of cervical cancer (76.7% of the cases in India).7 HPV vaccines are licensed in 100 countries and are a part of school vaccination programs in 58 countries including the neighboring country Bhutan where the government is providing the vaccine free of cost to 6th grade girls and look to achieve an immunization rate of over 90%. It is high time that we stop ignoring this highly prevalent, deadly yet completely preventable cancer. The vaccine has to be delivered prior to exposure to the HPV virus as it is a prophylactic vaccine, therefore, the immunization must precede the sexual debut. Evidence suggests the age for initiation for vaccination to be 10-12years, however, catch up vaccination can be done till 26years of age Figure 1&2.
|
Figure 1 WHO/ICO information centre on HPV and cervical cancer (HPV information centre) in India. Summary report 2010 (Accessed on 5th July2010)). |
Hepatitis B:
India is a country of high endemicity with 300,000 new Hepatitis cases occurring each year.8 The number of HBsAg carriers in India has been estimated to be over 40 million and annually around 205,286 deaths related to chronic hepatitis occur.1 Primary liver cancer, called hepatocellular carcinoma, is the 5fth leading cause of cancer death in adults worldwide and third most common cancer in developing world settings.9,10 Adults in high risk groups of acquiring Hepatitis B are healthcare providers, those who require frequent blood, injectable drug users, people having multiple sexual partners, men who have sex with men and household contacts of Hepatitis B patients or carriers. All children and adolescents younger than 18years old and not previously vaccinated should receive the vaccine. Hepatitis B vaccination is also indicated for all unvaccinated adults at risk for HBV infection and all adults seeking protection from HBV infection including post-exposure prophylaxis.1 Three doses (for high-risk groups if not previously immunized) are recommended.
Even healthcare providers who are at such a high risk of acquiring blood-borne infections like hepatitis-B have a low coverage of Hep -B vaccination amongst them. Influenza The burden of influenza or simply flu in adults is unimaginable as a study has revealed that during peak periods of influenza activity circulation i.e. during the monsoon period, 20% of all hospital admissions have influenza positivity.11 Around 40,000 deaths occur due to Influenza annually8 and the situation is grimmer when an epidemic or outbreak is there. A study from south India reported a monthly incidence of respiratory infections to be 23% in urban areas and 17.7% in rural areas among the paediatric age group.1Children might be having the highest infection rate but persons aged over 65years, young children and persons of any age who have some co-morbid medical conditions are at highest risk for complications, hospitalizations and deaths from influenza.CDC recommends administering inactivated influenza vaccine to all persons 6 months of age and older annually, however Indian Academy of Paediatrics (IAP) has recommended seasonal influenza vaccine to high risk children and adults like people with chronic cardiac, pulmonary (excluding asthma), hematologic and renal (including nephrotic syndrome) condition, chronic liver diseases, diabetes mellitus, acquired immunodeficiency (including HIV infection) and laboratory personnel and healthcare workers.
Hepatitis A:
The virus has a worldwide distribution and causes about 15 million cases of clinical hepatitis each year.1 Studies in India have shown HAV sero-prevalence to be between 38% to 92% in-different age groups.1 Various findings have shown that a significant proportion of the Indian adolescent and adult population is at risk of Hepatitis A Virus (HAV) infection. A study showed an increased incidence of symptomatic HAV among children (10.6% to 22.0%) and also in adults (3.4% to 12.3%) amongst the patients with acute viral hepatitis attending a hospital.12 Vaccine is specially recommended in high risk groups like international travelers, men who have sex with men, people with clotting factor disorder and persons with chronic liver disease.
Meningococcal disease:
Several major epidemics of meningococcal disease have been reported, pre-dominantly from the major cities, and particularly from New Delhi. This distribution may be because of over- crowding, vulnerability to the new strains, or suitable climatic conditions. Routine vaccination of the population at large is not recommended except during epidemic situations. Also, Meningococcal vaccine is recommended to be given to Haj pilgrims and other travelers visiting the countries where meningococcal disease is a major problem or where outbreaks are occurring and high-risk groups, e.g. children living in orphanages, jail inmates, soldiers in Barracks etc.
Chicken pox:
Many studies have found out that though chicken pox is a disease of children but in tropical countries like India, the disease is common in adolescents and adults in whom it causes greater morbidity and mortality. Due to reasons not clearly known, the sero-conversion in tropical countries is low leading to such a disease trend. The bigger problem that India is facing is that due to these factors, a large proportion of women of childbearing age are susceptible to Varicella Zoster virus during pregnancy. They may pass the virus to their unborn child leading to congenital varicella syndrome in the child. Vaccination may limit the morbidity and mortality associated with adult and neonatal disease and helps to reduce the individual, social and economic incurred by this dis-ease.
Shingles (Herpes Zoster):
Shingles is a painful and debilitating condition that occurs in elderly due to the chicken pox virus that lays dormant foryears in the nerve roots of spinal cord after causing chicken pox in childhood. One-fifth of childhood chickenpox infection leads to shingles in old age. Thus, it is important for people more than 60years to get this vaccine.
Pneumococcal Disease:
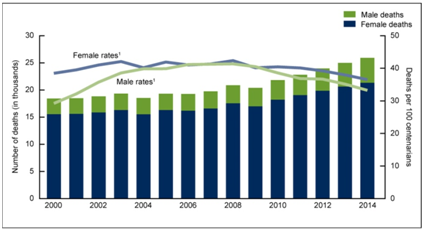
Preventable Invasive Pneumococcal Disease (IPD) includes meningitis, pneumonia and septicemia. They lead to great morbidity and mortality in all age groups worldwide. Around 85% of invasive pneumococcal disease occurs in adults. Among adults, with Community Acquired Pneumonia (CAP) requiring hospital admission, S pneumonia ranks first as a cause and accounts for most of such cases. There are 155.8 million clinical episodes of pneumonia globally, which contribute to approximately1.9million deaths, 70% of which occur in Africa and south-east Asia. ACIP recommends pneumococcal vaccination for the following adults: Age 65years and older, age 19-64years of age with: asthma, diabetes, lung, heart, or liver disease, or alcoholism, cigarette smokers and residents of long-term or chronic care facilities (e.g., nursing homes). A 23-valent vaccine is recommended in adults and prevents about 60-70% of the invasive disease. As shown in the Figure 3 below, death ratio between male and female (number of death and death rates) from 2000 to 2014 showing a linear increase from 2000 to 2008 and decrease from 2008 to 2014are statistically significant at p<0.05 level.
Roadblocks in adult vaccination
The reasons for low adult vaccination coverage are many. Adults are busy and ignore their health status for too long. Many adults do not go to the doctor regularly, or do not have a primary care physician. They just visit a physician when they fall ill or things go out of hand. Their priority is mostly getting short-term relief and they do not think about long-term health gains. There is a major lacuna in adult awareness about vaccinations and adults think that vaccination is only for kids. In an unpublished survey, it was found that more than 80% of the adults being surveyed did not know about adult vaccination. Additionally, there are no recommendations of vaccinations by family physicians as they them-selves have little awareness about the same. It is possible as there are no recommendations and guidelines for adult immunization in India and very few physicians recommend their adult patients any vaccines. There are lot of doubts in the minds of doctors and general public regarding the safety, efficacy and need of adult vaccines.
Way Forward
It has been more than three decades since Expanded Program on Immunization (EPI) was launched in India in 1978, and immunization has been further up scaled with introduction of Universal Immunization Program (UIP) in 1985. Since then, major strides have been taken to reach the vulnerable and eliminate the diseases. The infrastructure, manpower, and resources - all are in place and India should think of reaching the adults with vaccination too. The WHO scientific advisory group of experts (SAGE) to Global Program for Vaccines and immunization (GPV) has also indicated the need to expand immunization activities beyond infancy, either as part of routine immunization services, or as part of disease elimination and/ or eradication measures.1 Efforts should be made to increase awareness about adult vaccination so that the demand for the same increases. Private and general practitioners should seek opportunities to make their patients aware about adult vaccination, as healthy adults are difficult to target and reach. Lessons can be learnt from successful vaccination program in which pregnant females have been immunized against tetanus. This has led to the successful elimination of neonatal tetanus in India. Such an organized approach should also be replicated for other vaccines for adults. Political will is very important for any health program to be successful, so the government should make adult vaccination a priority and should ensure uninterrupted funding for the same. Last but not the least, research and development is imperative and a proper surveillance system should be in place so that the missing data can be found and a more solid ground is laid for adult vaccination in the country.13‒19
Conclusion
To conclude this article, reason behind is to generate awareness amongst the society, globally for adult vaccination. Adult vaccination to be taken up as a prime focused program as a part of Preventive Care. During 27years of my practice, I have diagnosed many patients with varieties of diseases which could have been prevented with vaccination during their adult age.
Acknowledgements
None.
Conflict of interest
Author declares that there is no conflict of interest.
References
- Monthly Newsletter of National Centre for Disease Control 1. Directorate General of Health Services, Government of India Adult Immunization. 2011;14:22.
- John S. Adults too need to get vaccinated. Sunday times 2. of India. 2008;27:29
- Sharma SK, Singal RK, Aggerwal AK. Adult Immunization (monograph). In: A publication of the Association of Physicians of India; 2009:1‒192.
- Ethics and the Vaccine Controversy
- Center for Disease Control and Prevention. Workplace health Promotion. Adult immunization.
- Serum Institute of India Ltd. Health FAQ Rubella.
- Kaarthigeyan K. Cervical cancer in India and HPV vaccination. Indian J Med Paediatr Oncol. 2012;33(1):7‒12.
- Gwalani P. Doctors call for national adult immunization drive. The Times of India; 2015.
- Parkin DM, Bray F, Ferlay J, et al. Estimating the world cancer burden: Globocan 2000. IntJ Cancer. 2001;94(2):153‒156.
- Pisani P, Parkin DM, Bray F, et al. Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer. 1999;83:18‒29.
- Chadha MS, Hirve S, Dawood FS, et al. Burden of seasonal and pandemic influenza-associated hospitalization during and after 2009 A (H1N1) pdm09 pandemic in a rural community in India. PLoS One. 2013;8(5):e55918.
- Hussain Z, Das BC, Husain SA, et al. Increasing trend of acute hepatitis A in north India: need for identification of high-risk population for vaccination. J Gastroenterol Hepatol. 2006;21(4):689‒693.
- Williams WW. Adult vaccination update. Advisory Committee on Immunization. Center for Disease Control. Atlanta, USA;
- Essential vaccines.
- Larry M, Baddour MD. Whole virus H5N1 vaccine trial. Journal Watch Infectious Diseases. 2008:6.
- Vijayakumar V, Hari R, Parthiban R, et al. Evaluation of immunogenicity and safety of Genevac B: a new recombinant hepatitis B vaccine in comparison with Engerix B and Shanvac B in healthy adults. Indian J Med Microbiol. 2004;22(1):34‒38.
- Citation: Rathi A, Sharma S. Vaccine Preventable Diseases in Indian Adults-Burden & Prevention. Infect Dis Diag Treat. 2017;2017:J102.
- Rathi A, Garg S, Meena GS. Human Papillomavirus Vaccine in Indian Settings: Need of the Hour. J Vaccines Vaccin. 2016;7:346.
- Singhal V, Bora D, Singh S. Hepatitis B in health care workers: Indian scenario. J Lab Physicians. 2009;1(2):41‒48.