Volume : 4 | Issue : 1
Case Report
Treating the atrophic maxilla with four, three, or even one ultrashort implant
Rolf Ewers,1 Mauro Marincola,2 Paolo Perpetuini3
1 University Hospital for Cranio-Maxillofacial and Oral Surgery, Austria
2Implant Dentistry Center University of Cartagena Colombia
3Dental Technician, Laboratorio Odontotechnico, Italy
Received: April 11, 2021 | Published: May 18, 2021
Abstract
In continuation of the prospective cohort study of patients with a class V or VI severely atrophic maxilla treated with four ultrashort 4.0 x 5.0 mm locking taper conus implants, now, a study of patients is presented with more severely atrophic maxillae. The use of only three 4.0 x 5.0 mm, 4.5 x 5.0 mm, or 4.5 x 6.0 mm ultra-SHORT® Implants, is the significant difference of this new study. The use of one implant placed through the incisive foramen and into the nasopalatine canal makes these treatments possible. The implants were restored with prostheses fabricated with the CAD/CAM, metal–free, fiberglass reinforced hybrid resin material, TRINIA®. The implant insertions did not cause any sensorial nerve disturbances. Since the three-implant restorations successfully supported twelve–unit fixed prostheses, a third study was initiated using only one implant with an overdenture fabricated with the new resin reinforced metal free material and retained with a Brevis abutment.
Keywords: Reduce the number of implants, reduce the size of implants, locking taper and conus implants, extreme maxillary atrophy, alveolar crest splitting, avoiding sinus elevation procedures, avoid augmentation procedures, metal–free fiberglass–reinforced hybrid resin prostheses, fabrication of CAD/CAM prostheses, overdentures on one implant, triangular–stability.
Introduction
Rehabilitation of the severely atrophic maxilla is always an incredibly challenging task for both surgical and prosthetic clinicians. The early loss of the dentition and long lasting edentulism lead to atrophy throughout the maxilla. Especially, the early loss of molars leads to a significant atrophy of the alveolar process and an extensive pneumatization of the maxillary sinus.1 Since Tatum’s lecture about the so-called “sinus lift”,2 many methods have been reported to solve these problems with excellent long-term results.3–8 With more experience and treatments being performed, these procedures became minimally invasive.9–11 As Osseointegration has been defined as a direct and functional connection between bone and an artificial implant12 time has proofed that function is also important for a long lasting osseointegration besides implant material and coating.13 Therefor in the last three decades short and ultrashort implants have become more commonly used as an alternative to conventionally long implants in conjunction with bone augmentation procedures. And yet, scientifically evidenced–based reports are still few - especially for the severely atrophic edentulous patient, who is one of the most challenging patients for dentists to provide implant prostheses.
To avoid extensive surgical vertical and horizontal augmentation procedures, such as sinus lifts, in 2010 a prospective cohort study was initiated at the University Hospital with four 4.0 x 5.0 mm, posteriorly placed implants. When thin anterior alveolar ridges necessitated, 3.0 x 8.0 mm calcium phosphate–coated (CP) locking taper implants14 were placed. In complex cases it was observed that the options for augmentation and implant placements in the anterior maxilla were extremely limited due to the narrow width and limited height of the alveolar crest. Therefore, currently there is a prospective cohort study with three ultrashort 4.0 x 5.0 mm CP coated locking taper implants for the severely atrophic maxilla in concert with the longer existing study of three ultrashort implants in the mandible.15 Depending on the size and form of the incisive foramen and nasopalatine canal,16 4.5 up to 6.0 mm diameter ultrashort implants were used.17 To determine if it would be possible to insert an ultrashort implant into the incisive foramen and the nasopalatine canal, a preoperative Cone–Beam Computed Tomography (CBCT) is essential.18–20
The middle ultrashort implant is inserted into the incisive foramen and nasopalatine canal, where there is usually one cavity with two nerves,21 since this is the thickest boney site in the atrophic premaxilla where an implant can be placed. Most incisive foramen have one cavity in which two incisive nerves are situated.22–24 For Le Fort I Osteotomies25 and for Horseshoe Le Fort I Osteotomies with free Iliac crest bone block transplants,26,27 the incisive nerve and vessel structures are always cut without any permanent clinical effects. This fact is also true for the placement of an implant into the nasopalatine canal, despite most authors denying this fact.28 De Mello et al.29 have shown in a large–scale systematic review and meta–analysis of 238 articles, where they cited ten articles with references to 91 implants being inserted into the incisive foramen with a success rate of 84.6 % to 100 %, with only one permanent nerve disturbance being reported after the lateralization of the nerve. For all the twelve–unit full arch implant loaded prostheses,30 TRINIA®, a metal–free, fiber–reinforced hybrid resin CAD/CAM material was used.
Previously, for most severely atrophic maxillae, a Horseshoe Le Fort I Osteotomy with a free iliac crest bone transplant was performed.27 However, after the favorable results reported by Kern31 and others32 treating the mandible with only one implant, a small series was started to try to perform this method also in the maxilla, inserting one ultra-SHORT® implant into the incisive foramen and nasopalatine canal to enable an overdenture on a single Brevis™ abutment.
Materials and methods
This “prospective cohort study” was approved by the institution’s ethical committee under the number “EK 018/2011” The prospective study was designed according to the Declaration of Helsinki, as well as the Good Clinical Practice guidelines. The study is designed as a bicentric cooperation between the University Hospital for Cranio–Maxillofacial and Oral Surgery Vienna and the CMF Institute Vienna.
Consecutively, all edentulous patients with pronounced maxillary atrophy Class V and VI according to Cawood and Howell,33 in consideration of the common criterion of exclusion and after a written consent were included. Patients with Bisphosphonate/Denosumab–anamnesis, heavy smokers with more than 10 cigarettes per day and adolescents were excluded.
Study No. I with four implants
All 18 patients, 54 to 80 years of age (12 women; mean age, 66.9±9.0 year; range, 54.0 to 79.7 year; 6 men; mean age, 67.6±5.3 year; range, 61.4 to 76.5 year; there was no significant age difference between female and male patients) had been treated with four 4.0 x 5.0 mm ultra–SHORT® Implants, covered with Integra–CP® surface (Bicon, Boston, USA), For patients with very thin maxillary anterior alveolar crests, 3.0 x 8.0 mm locking taper implants were placed.17,34 The healing time for the implants was six months. During the uncovering session, the impressions and the bite registration were made. For the prosthetic rehabilitation, a 12–unit full–arch CAD/CAM produced prosthesis fabricated with TRINIA® metal–free fiberglass–reinforced hybrid resin material was used, which was either cemented onto the abutments or attached with screws and fixed–detachable abutments. After finishing their prosthetic treatment, patients had been evaluated yearly in a recall program, which included panoramic radiographs.
Materials and methods
This “prospective cohort study” was approved by the institution’s ethical committee under the number “EK 018/2011” The prospective study was designed according to the Declaration of Helsinki, as well as the Good Clinical Practice guidelines. The study is designed as a bicentric cooperation between the University Hospital for Cranio–Maxillofacial and Oral Surgery Vienna and the CMF Institute Vienna.
Consecutively, all edentulous patients with pronounced maxillary atrophy Class V and VI according to Cawood and Howell,33 in consideration of the common criterion of exclusion and after a written consent were included. Patients with Bisphosphonate/Denosumab–anamnesis, heavy smokers with more than 10 cigarettes per day and adolescents were excluded.
Study No. I with four implants
All 18 patients, 54 to 80 years of age (12 women; mean age, 66.9±9.0 year; range, 54.0 to 79.7 year; 6 men; mean age, 67.6±5.3 year; range, 61.4 to 76.5 year; there was no significant age difference between female and male patients) had been treated with four 4.0 x 5.0 mm ultra–SHORT® Implants, covered with Integra–CP® surface (Bicon, Boston, USA), For patients with very thin maxillary anterior alveolar crests, 3.0 x 8.0 mm locking taper implants were placed.17,34 The healing time for the implants was six months. During the uncovering session, the impressions and the bite registration were made. For the prosthetic rehabilitation, a 12–unit full–arch CAD/CAM produced prosthesis fabricated with TRINIA® metal–free fiberglass–reinforced hybrid resin material was used, which was either cemented onto the abutments or attached with screws and fixed–detachable abutments. After finishing their prosthetic treatment, patients had been evaluated yearly in a recall program, which included panoramic radiographs.
Materials and methods
This “prospective cohort study” was approved by the institution’s ethical committee under the number “EK 018/2011” The prospective study was designed according to the Declaration of Helsinki, as well as the Good Clinical Practice guidelines. The study is designed as a bicentric cooperation between the University Hospital for Cranio–Maxillofacial and Oral Surgery Vienna and the CMF Institute Vienna.
Consecutively, all edentulous patients with pronounced maxillary atrophy Class V and VI according to Cawood and Howell,33 in consideration of the common criterion of exclusion and after a written consent were included. Patients with Bisphosphonate/Denosumab–anamnesis, heavy smokers with more than 10 cigarettes per day and adolescents were excluded.
Study No. I with four implants
All 18 patients, 54 to 80 years of age (12 women; mean age, 66.9±9.0 year; range, 54.0 to 79.7 year; 6 men; mean age, 67.6±5.3 year; range, 61.4 to 76.5 year; there was no significant age difference between female and male patients) had been treated with four 4.0 x 5.0 mm ultra–SHORT® Implants, covered with Integra–CP® surface (Bicon, Boston, USA), For patients with very thin maxillary anterior alveolar crests, 3.0 x 8.0 mm locking taper implants were placed.17,34 The healing time for the implants was six months. During the uncovering session, the impressions and the bite registration were made. For the prosthetic rehabilitation, a 12–unit full–arch CAD/CAM produced prosthesis fabricated with TRINIA® metal–free fiberglass–reinforced hybrid resin material was used, which was either cemented onto the abutments or attached with screws and fixed–detachable abutments. After finishing their prosthetic treatment, patients had been evaluated yearly in a recall program, which included panoramic radiographs.
Results
Of the 18 patients with 72 implants which were previously reported,14 only 12 patients are still remaining in the recall program, due to severe illnesses or demise. The longest evaluation is 98 months (8.2 years). For the 48 implants inserted in these 12 patients, 4 implants have been lost (8.33%). The four patients who lost an implant, were able to function on their three remaining implants until the fourth one was replaced. There have been no observed fractures of the 12 TRINIA® prostheses. As previously reported,17 radiographs reveal only slight marginal bone loss.
Case reports
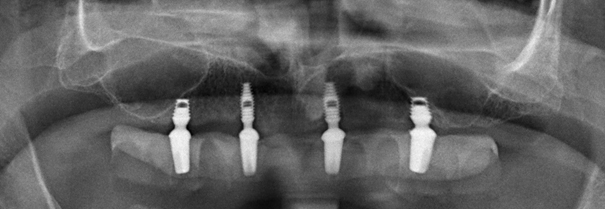
As an example, an already published treatment of a 69-year-old male patient,12 who last presented for his 6–year recall is being presented. The panoramic radiograph shows in Figure 1A his initial situation, and Figure1b his situation at time of loading. Initially, the patient had a cemented prosthesis on four abutments. Later the patient asked to have a removable telescopic solution, which Figure 1C shows after his 6 years of loading.

|
Figure 1A Magnified section of a panoramic radiograph of a 69-year-old male patient with extensive maxillary atrophy with a splint and two metal points incorporated for navigation help. |

|
Figure 1B Magnified section of a panoramic radiograph with four inserted 4.0 x 5.0 mm SHORT® Bicon Integra CP implants cemented on four abutments. |

|
Figure 1C Magnified section of a panoramic radiograph with a TRINIA® prosthesis fixed on four individually milled telescopic abutments and copings after 6 years of loading. |
Figures 2a and 2c show the intraoral view after 6 years. Note on this image the new telescopic prosthesis with four individually milled telescopic abutments and copings, which accommodated the patient’s request after 4 years for a full-arch removable prosthesis with short distal extensions (Figure 2A-2C). The second demonstration is of a 69-year-old male patient, who had not only a pronounced maxillary atrophy class V–VI.33 in vertical dimension, but also a very thin alveolar process in the premaxilla and premolar region. Therefore, bilaterally in the frontal region a 3.0 x 8.0 mm SHORT® implant was placed. For the very narrow alveolar crests in the premolar region, after a supra–periosteal tissue preparation and a widening or spreading of the alveolar crest, were performed before inserting the 4.0 x 5.0 mm ultra–SHORT® implant. The panoramic radiograph in Figure 3A shows his initial situation, Figure 3B at time of loading and Figure3c at his 6–year recall. Figure 4 shows the situation intraorally after six years of loading.

|
Figure 2B Undersurface of the TRINIA® prosthesis with four individually milled telescopic copings and short extensions since distal implants could not have been inserted more posteriorly. |

|
Figure 3A Magnified section of a panoramic radiograph of a 69-year-old male patient with pronounced class V-VI maxillary atrophy. |
|
Figure 3C Magnified section of a panoramic radiograph after six years of loading, revealing no marginal bone loss. |
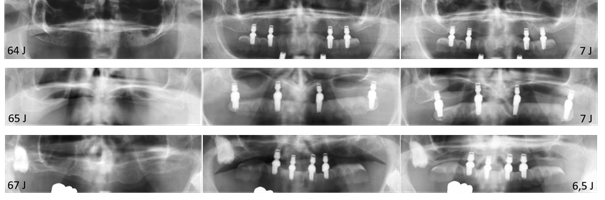
Concluding the presentation of four Bicon implants panoramic radiographs of implants with 6.5 and 7 years of loading is shown (Figure 5). On the left side is their preoperative images, in the middle is their images at initial loading, and on the right side is their latest recall radiograph. Images in the upper row are of a 64-year-old female patient with 7 years loading, images in the middle row are of a 65-year-old female also with 7 years of loading and images in the lower row are of a 67-year-old male with 6.5 years of loading.
Interestingly, there always appears to be a visible stability of the bone levels around the implants. Although all the implants are splinted and are not individually loaded, there is no peri–implant bone loss visible.
Study No. II with three implants
Eleven patients aged between 55 to 86 years old with extreme maxillary atrophy class V to VI according to Cawood and Howell33 were included in this study group. All patients had been treated with a 4.0 x 5.0 mm implant on each premolar side and a 4.5 up to 6.0 mm diameter calcium phosphate coated ultra–SHORT® implant in the incisive foramen and nasopalatine canal.15,17,34 In very thin premolar regions, an alveolar crest widening or splitting procedure after a supra–periosteal preparation was performed.35 The anatomical peculiarities and the special operative techniques have been previously described.34 The healing time for the implants was six months. The prosthetic rehabilitation was with a 12–unit full–arch CAD/CAM produced prosthesis fabricated with metal–free fiberglass–reinforced hybrid resin material.
Results
Of the eleven patients with 33 implants, six were women (58.2 to 68.7 years) and five were men (63.4 to 81.6 years). They all had been in a twice per year recall regimen. The mean observation period is 34.2 months, and the longest observation period is 66 months (5.5 years). In the premolar region twenty–two calcium phosphate coated locking taper Integra–CP implants were placed. For the incisal foramen and nasopalatine canal, four 4.5 x 6.0 mm, four 5.0 x 6.0 mm and three 5.0 x 5.0 mm calcium phosphate coated locking taper Integra–CP implants were placed. During the observation period of 5.5 years, all implants remained osseointegrated and only two implants (6.06 %) were lost.
The loss rate is relevant considering the following: the advanced age of both patients, the extreme maxillary atrophy, the relatively large diameter of incisive foramen and nasopalatine canal, and the surgeon’s experience with the new surgical placement techniques. The wider the foramen, the more difficult it is to insert an implant. Surprisingly, both patients were able to use their prosthesis very carefully on only two implants, during the osseointegration time of their replacement implant. None of the 11 twelve–unit prosthesis showed any fracture of the resin material. As reported with four implants,14 there were only minor changes in the marginal bone levels with three implants.
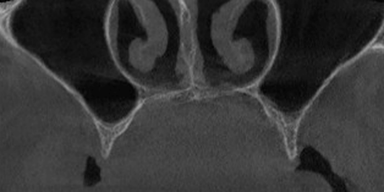
Case report
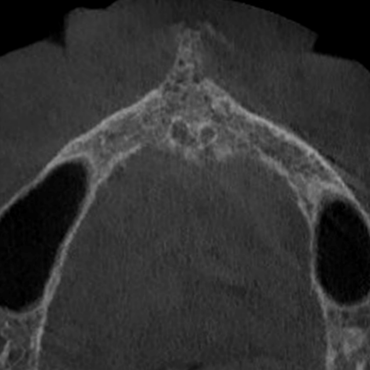
The treatment of 65-year-old patient, which was previously reported17 presented at his 4–year reevaluation is being shown. Figure 6a shows a Cone Beam CT in transvers projection before extraction of his teeth 6 through 10 with massive lone loss around the teeth. Figure 6B reveals the severe bone defect of premaxillary bone. Only around the incisive foramen and the nasopalatinal canal is bone left. Figure 6c shows the insertion of three implants. Figure 6d shows the Cone Beam CT in sagittal projection after insertion of the middle Bicon implant through the incisive foramen and into the nasopalatine canal.

|
Figure 6A Cone Beam CT in transverse projection revealed massive bone loss around teeth 6 through 10 prior to their being extracted. |

|
Figure 6B Cone Beam CT in transverse projection after extraction of the teeth, reveals extensive bone loss, except for an area around the nasopalatine canal where there is some remnant bone. |

|
Figure 6D Cone Beam CT in sagittal projection after inserting the middle Bicon implant through the incisive foramen into the nasopalatinal canal. |
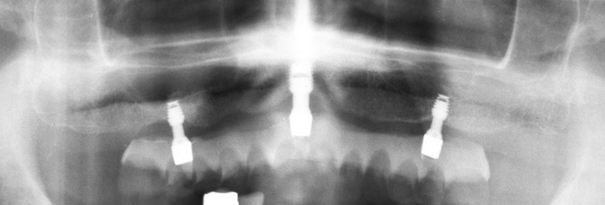
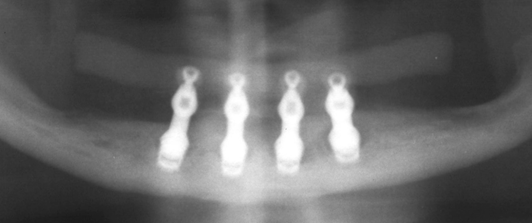
Figure 7A shows a section of a panoramic radiograph at initial loading with the prosthesis onto the three fixed detachable abutments. Figure 7B the appearance at the 4 year recall visit. Note: there is no apparent change of marginal bone level around the Bicon implants. Figure 8 shows the intraoral situation at his 4–year recall.

|
Figure 7A Section of a panoramic radiograph at initial loading with the TRINIA® prosthesis onto the three fixed-detachable abutments. |
|
Figure 7B Section of a panoramic radiograph with screw retained full arch TRINIA® prosthesis on three fixed-detachable abutments at the 4-year recall. |
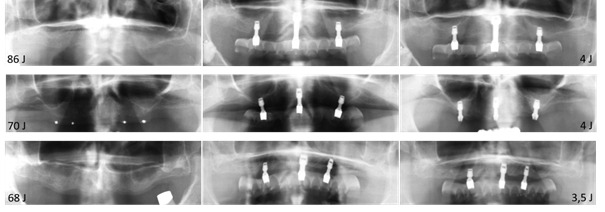
Concluding the reporting of the study with three implants, a panoramic radiograph survey of three patients with 4- and 3.5-years loading time is being shown (Figure 9). On the left side are images before the implant’s insertions. In the middle column at their initial loading, and on the right side at their last recall. In the upper row is an 86-year-old female patient (one of the oldest) with a 4–year loading, in the middle row a 70-year-old male patient also with a 4–year loading, and in the lower row a 68-year-old female patient with a 3.5–year loading. Interestingly, there always is a visible stability of the bone levels around the implants. Although all implants are splinted and not individually loaded, there is no peri–implant bone loss visible.
Study No. III with one implant
Based on the gained experience and the successful results of the studies with “all–on–four” and “all–on–three” (and according to the suggestions and reported good results in the mandible by Kern et al.31), it was decided to try to insert only one ultra–SHORT® implant in the maxilla through the incisive foramen into the nasopalatine canal to support a TRINIA® overdenture in the atrophic maxilla. Proportionally to the width of the nasopalatine canal, an ultrashort Bicon implants with diameters up to 6.0 mm were used.
Results
On four patients ages of 62 to 75 years, implants were inserted through the incisive canal and into the nasopalatine canal. The implants used ranged from a 4.5 mm up to 6.0 mm x 5.0– and 6.0 mm calcium phosphate coated locking taper implants with a healing time of six months. The prosthetic rehabilitation was with a full–arch CAD/CAM produced prosthesis fabricated with the metal–free fiberglass–reinforced hybrid resin material. The prostheses were fixed to a single implant with a Brevis™ (Bicon) attachment and abutment. During the short observation period of 30 months, no complications were observed, and all patients are incredibly happy with their prosthetic solution. Importantly, the patients have the feeling that their prosthesis is not loose and not in danger of inadvertently slipping out of their mouth – despite their extreme maxillary atrophy.
Case report
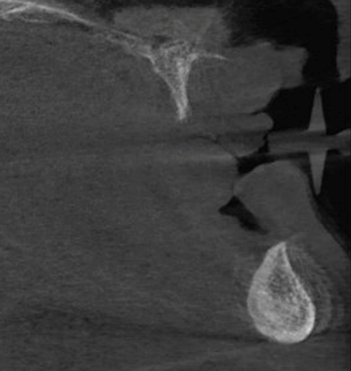
For a 75-year-old female patient, diagnosed with an extreme maxillary atrophy class VI (Figure 10A & B) and a mild mandibular atrophy class III–IV33 (Figure 10C) after being edentulous for 57 years.
The only region of the maxilla with sufficient bone for an implant is the premaxilla with two incisive foramina and nasopalatine canal in the middle (Figure 10D).

|
Figure 10A Panoramic radiograph of a 75-year-old female patient with extreme maxillary atrophy class VI and a mild mandibular atrophy class III-IV [33] after being edentulous for 57 years. |
|
Figure 10B Frontal section of a Cone Beam CT with extreme bilateral atrophy of the alveolar crests in the premolar region, class VI [33]. |
|
Figure 10C Sagittal Section of a Cone Beam CT showing an extreme progenic Angle class III bite relationship. |
|
Figure 10D Transverse section of a Cone Beam CT showing the premaxilla with two incisive foramina and the nasopalatine canal. |
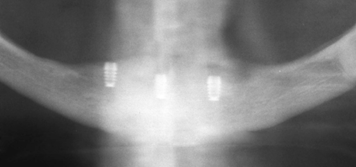
Initially, the mandible was treated by inserting three 4.0 x 5.0 mm Bicon CP coated locking taper implants (Integra–CP) (Figure 11A).
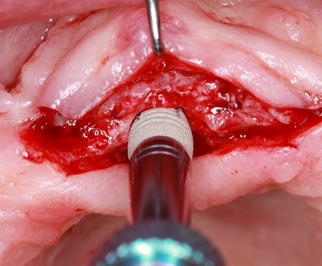
After two months one 5.0 x 6.0 mm CP coated locking taper implant was placed through the incisive canal and into the nasopalatine (Figure 11B).
|
Figure 11B Intraoperative view during the insertion of a 5.0 x 6.0 mm CP coated locking taper implant with the Implant Inserter/Retriever instrument on a Threaded Straight Handle. |
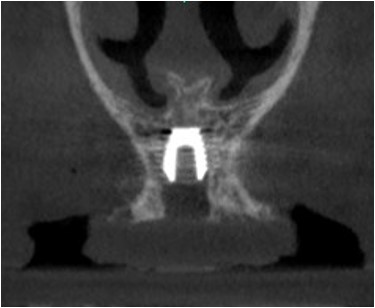
The postoperative Cone Beam CT images in Figures 12A and 12B reveal a satisfactory position of the implant in the premaxilla. During the six months of osteointegration of the maxillary implant, the mandibular implants were uncovered, and at the same session the impression and the bite registration were made. Note the facial position of the impression posts (Figure 13).
|
Figure 12A Frontal section of a Cone Beam CT after insertion of a 5.0 x 6.0 mm Bicon CP coated locking taper implant. |

|
Figure 12B Sagittal section of a Cone Beam CT after inserting a 5.0 x 6.0 mm Bicon CP coated locking taper implant. |

|
Figure 13 Intraoral image after the uncovering the implants and insertion of the impression posts. The too facially positioned impression posts reveal progenic (Angle class III) situation. |
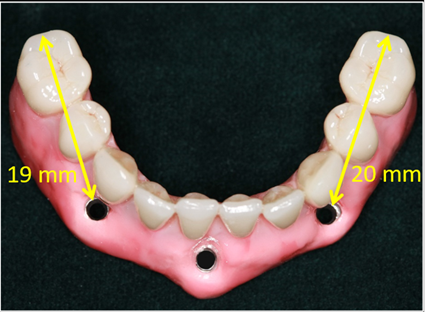
After the Perpetuini Dental Laboratory had fabricated the full–arch CAD/CAM prosthesis with metal–free fiberglass–reinforced hybrid resin material, the problem of the too facially positioned implants due to the progenic class III malposition was solved. The three sleeves and screws were positioned in front of the canines and incisors (Figure 14 & 15).
The position of the fixed–detachable abutments (Figure 16) clearly reveals an extreme progenic class III malocclusion. Figure 17 shows the full–arch prosthesis fixed with three screws in the screw detachable abutments. Figure 18 reveals the long bilateral extensions (cantilevers) due to the extreme labial positioning of the screws. The entire prosthesis is a distal extension (cantilever).

|
Figure 16 Intraoral situation after inserting the fixed-detachable abutments to the three Bicon implants. The extreme progenic class III position is clearly evident. |
Ten years ago, the authors experienced facially positioned implants in a progenic class III relationship for a 59-year-old female patient, whose four 4.0 x 5.0 mm CP coated locking taper implants had been tilted too far labially (Figure 19B). Their position necessitated that the sleeves and screws be positioned far in front of the canines and incisors. The panoramic radiograph (Figure 19A) reveals the exceptionally long extensions (cantilevers). Left is 21.0 mm and the right 19.0 mm. Once again, the entire prosthesis is a distal extension (cantilever).

|
Figure 18 Section of a panoramic radiograph after fastening the full-arch prosthesis with three screws, revealing long bilateral extensions (cantilevers). |
The lateral cephalometric radiograph also reveals the distinctly long bilateral extensions (cantilevers) of 21.0 mm on the left side and 19.0 mm on the right side of the prosthesis (Figure 19B).
Figure 20A shows the intraoral situation at the 9–year recall revealing the successful resolution of the facially angled implants. Despite the extreme loading during the 9 years of prosthetic wear, there was no fracture of the prosthesis and no apparent bone loss visible on the panoramic radiographs (Figure 20B).
|
Figure 20B Section of panoramic radiograph taken at more than 9-years loading. No peri-implant bone loss is visible. |
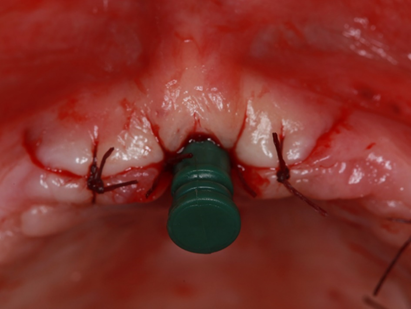
Continuing with the discussion above, a 75-year-old female patient, whose implants were uncovered after six months is presented. During the same session, the impressions and the bite registration were made (Figure 21). A few days later, another bite registration was made at the try–in session with the prepared overdenture base providing fixation for the orientation. The green plastic impression sleeve fits precisely onto the titanium impression post to ensure a precise try–in and bite registration (Figure 22).
|
Figure 21 Intraoral situation with plastic impression sleeve fixed over the titanium impression post after uncovering the implant for immediate impression taking and bite registration. |

|
Figure 22 Prepared overdenture prosthesis being used as fixation and orientation for the try-in and the bite registration. |
Image of the finished prosthesis, which was fabricated by Paolo Perpetuini. Figure 23 shows the single Brevis™ attachment fixed in the implant analog of the master model. Figure 24 shows the finished prosthesis and Figure 25 the prosthesis from below with the Brevis™ attachment in the middle.

|
Figure 25 Finished TRINA® overdenture prosthesis from below with the Brevis™ attachment in the middle. |
Despite the class III bite relationship due to the extensive maxillary and mandibular atrophy, it was possible to achieve an adequate overjet and overbite by increasing the vertical dimension (Figure26). Lateral image confirms the result (Figure 27).
Figures 28& 29 reveal a very satisfied patient with an aesthetic appearance with only a slight progenic chin.
According to the patient’s opinion, she has been given a very satisfactory functional and aesthetic result. She can chew her food without any difficulties, since her upper prosthesis does not wiggle anymore and keeps its position securely in her mouth.
Discussion of the study groups with four, three and one implant
The aim of this study was to investigate the possibility of treating patients with extreme maxillary atrophy by means of short and ultrashort implants, without the necessary time and cost of intensive augmentation procedures and to minimize the morbidity and complication risks of using augmentation procedures. The full-arch prostheses were CAD/CAM produced out of TRINIA®, a metal–free glass fiber reinforced hybrid resin material and were fixed on 4.0 x 5.0 mm and 3.0 x 8.0 mm ultra–SHORT® implants. The implant-based survival rate with a surveillance time of up to 8.2 years was 91.67%. These survival rates are comparable with the survival rates of standard long implants – especially if you take into consideration that all the presented patients showed a pronounced maxillary atrophy and were elderly. This study shows that it is possible to treat the very atrophic maxilla of elderly patients with the “all–on–four” concept with four ultrashort and narrow diameter Bicon implants.13,36–41 These results are comparable with reports about standard long implants of other authors.39–42 After two years of experience, cemented prostheses were substituted with screw–retained prostheses, which are also recommended by the S3 guidelines.43 For the prosthetic rehabilitation with four implants, the focus was on providing a precise occlusal rehabilitation with the opposing jaw. A centric premolar and molar occlusion with minimal or no anterior contact was always sought. For eccentric movements, canine guidance or group guidance was sought. Additionally, steep inclinations were avoided. Furthermore, emphasis on the curve of Spee to achieve a balanced axial loading of the implants was always a goal. When treating patients with severe maxillary atrophy with a new prosthesis one must emphasize a correct vertical dimension of occlusion, for it is highly likely that it has been reduced due to the loss of teeth, with subsequent repositioning of the joint. Increasing the vertical dimension of occlusion may improve the Angle class III relationship, which many long–term edentulous patients with massive jaw atrophy have. Due to the advanced age of the patients, it is easier for them to clean a removable prosthesis than a fixed, because of their compromised tactile visual capabilities. Furthermore, the study has shown that treating patients with a CAD/CAM produced prosthesis fabricated with metal–free fiberglass–reinforced hybrid resin material did not show any complications.34 All four patients who had to wait for osseointegration of their replaced implant were able to use their prosthesis on three implants, which means a 100% prosthetic success. The results using short and narrow Bicon implants are encouraging for the treatment of the extremely atrophic maxilla without extensive augmentation procedures, which not only saves the patient time and money, but more importantly with less pain and morbidity.
Since the study of the atrophic maxilla with four ultrashort Bicon implants showed such good results,14,44–46 it was considered to use only three implants, contrary to the meta–analysis47 and the suggestions of the S3 guidelines.43 However, the treatment followed the principle of “triangular stability”. Initially the three-implant study started in the mandible without any problems48 and subsequently in the maxilla.34 To reduce the implant number to three in the maxilla however, one probably must insert the middle implant through the incisive foramen and into the nasopalatine canal. Due to the author’s many years of operating experience with the Le–Fort–I osteotomy25 and the Horseshoe–Le–Fort–I osteotomy,26,27 he knew this procedure would have no sensational disturbances of the incisive nerves. De Mello et al.29 confirms these observations in his review and meta–analysis report. The implant survival rates are comparable with the results of standard long implants in combination with augmentation procedures. The implant survival for up to 5.5 years is 93.94 %. This shows that it is possible to treat the highly atrophic maxilla with the concept of “all–on–three” with ultrashort Bicon implants.17,34,36,37 The studies are comparable with studies of other authors.44–46 Furthermore, this study also shows that the use of metal–free fiber–reinforced resin hybrid CAD/CAM prostheses did not show any problems or complications.34 These results are reassuring as they had to be performed in some cases with alveolar crest widening and splitting due to the extreme maxillary atrophy. By inserting the middle Bicon implant through the incisive canal and into the nasopalatine canal, wider implants were able to be used. The prosthetic treatments were performed in the same manner as for the patients with four implants. With the “triangular stability” there were fewer tilting effects on the abutments. Since ridge–lap prostheses require greater hygiene, it is better to use fixed removeable prostheses for elderly patients because of their compromised capabilities.
Due to the recommended and widely published method of Kern et al.31 and other positive reports about treating the mandible with only one implant,32 it was decided to use these novel concepts in the maxilla. The anecdotal evidence for an observation period of 28 months, without the loss of a single implant is far too short to discuss this treatment as a successful modality and certainly not to recommend it. However, the extreme satisfaction of the patients with a partially stable maxillary full–arch prosthesis with only one implant encourages the continued use of this method. Just consider the benefits of being able to properly masticate one’s food, which leads to healthy digestion and nutrition.
Referring to the review and meta–analysis of removable and fixed implant–supported prostheses in edentulous jaws47 and the systematic S3 guidelines,43 this report contributes to the long–discussed reduction of implant numbers to four implants and even to the use of only three implants.
Due to the locking taper Bicon implant system without a bacterial film at the implant abutments interface, no soft tissue problems or peri–implantitis were observed. Interestingly, in all of the panoramic radiographs there appears to be a visible stability of the bone levels around the implants. Although all of the implants were splinted and not individually loaded, there is no observed peri–implant bone loss visible. Probably, one explanation of this phenomenon is due to the fact that the TRINIA® material is flexible. The flexibility between the splinted implants during functional loading may be the beneficial factor according to Wolff’s law,49 which provided the accelerated mineralization and possible bone gain. Additionally, and notably, the flexibility of the TRINIA material, which by definition cannot be a lever or cantilever, provided the opportunity of using apparently excessively long distal extensions (cantilevers).
Conclusion of the three study groups
Initially in 2010, the author was very skeptical when he started to treat his patients with four ultrashort Bicon implants – even though the Bicon system had been widely used and phenomenally successful for 25 years by that time. Since there had been no reports about the use of 4.0 x 5.0 mm implants in very atrophic jaws, he started first in the mandible and, after seeing successful results, he continued with maxillary treatments. Considering the challenging anatomy of highly atrophic maxillae with minimal bone volumes and without complex and costly augmentation procedures, he can state that the initial use of four and subsequently three ultrashort Bicon locking taper implants shows after an extended observation period, equivalent results as standard long implants with complex augmentation methods. Additionally, implant placement in the incisive foramen and nasopalatine canal did not lead to any complication and seems to be a sound procedure.
The presented treatments contradict the S3 guidelines.43 Therefore, there should be discussions about the presented methods as a practical way of reducing the number of implants due to the excellent results shown. Additionally, successful use of narrower implants has been shown, which offer significant surgical benefits. The medium–term observations of more than 8 years in the maxilla and more than 10 years in the mandible are satisfactorily compelling, especially considering the advanced age of the studied patients with their evident difficulties with implant and prosthetic maintenance issues.50 We significantly exceeded the initial goal of enhancing the quality-of-life elderly patients. As a positive side effect, it must be mentioned that their improved mastication has provided for their having an improved and well–balanced nutrition. Furthermore, the good results seem not only be influenced by the learning curve of the operating surgeons.51 Reports concerning the long–term results with only three and four ultrashort implants are still scarce. Similar prospective studies with long observation periods are recommended. Much to the delight of needful patients, it seems practical to treat the very atrophic maxilla with only one implant for an implant–stabilized full–arch TRINA® prosthesis. However, further long–term studies are also recommended.
Acknowledgments
None.
Conflicts of interest
All four authors do not have any conflict of interests.
Authorships
Rolf Ewers: Author, who surgically treated most of the patients and prosthetically all the patients.
Mauro Marincola: Surgically treated some of the patients and advised about prosthetic treatments.
Paolo Perpetuini: Fabricated all the laboratory aspects of the prostheses.
Funding
Bicon Dental Implants, 501 Arborway, Jamaica Plain, MA 02130, United States provided advice and funding for implant and prosthetic components.
References
- Cavalcanti MC, Guirado TE, Sapata VM, et al. Maxillary sinus floor pneumatization and alveolar ridge resorption after tooth loss: a cross-sectional study. Braz Oral Res. 2018;32:e64.
- Tatum OH. Lecture presented to the Alabama Implant Congress. Alabama Implant Congress. 1976.
- Tatum H. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30(2):207–229.
- Summers RB. The osteotome technique: Part 3--Less invasive methods of elevating the sinus floor. Compendium. 1994;15:698,700,702–4passim,quiz710.
- Ewers R. Maxilla sinus grafting with marine algae derived bone forming material: a clinical report of long-term results. J Oral Maxillofac Surg. 2005;63(12):1712–1723.
- Ewers R. Standard clinical Situations - 4.7 Edentulous Maxilla. In: Ewers R, Lambrecht JT, editors. Oral Implants: Bioactivating Concepts. Chicago: Quintessence Publishing, 2012:329–356.
- Ewers R. Implant Surgery. In: Lambrecht JT. Oral and Implant Surgery: Principles and Procedures – Implant Surgery. Chicago: Quintessence Publishing, 2009:350–360.
- Esposito M, Grusovin MG, Felice P, et al. The efficacy of horizontal and vertical bone augmentation procedures for dental implants - a Cochrane systematic review. Eur J Oral Implantol. 2009;2(3):167–184.
- Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium 1994;15:152,154– 156, 158 passim; quiz 162.
- Ali SA, Karthigeyan S, Deivanai M, Kumar A. Implant reha- bilitation for atrophic maxilla: A review. J Indian Prosthodont Soc 2014;14:196–207.
- Pérez-Martínez S, Martorell-Calatayud L, Peñarrocha-Oltra D, et al. Indirect sinus lift without bone graft material: Systematic review and meta- analysis. J Clin Exp Dent. 2015;7:e316–e319.
- Ewers R, Marincola M, Morgan V, et al. Der atrophe Oberkiefer und seine Versorgungsmöglichkeiten mit vier ultrakurzen Implantaten. Implantologie. 2018;26(1):61–70.
- Schwartz SR. Short Implants. An Answer to a Challenging Dilemma? In: Dym H, editor. Surgical and Medical Management of Common Oral Problems. Dental Clinics of North America. 2020;64(2).
- Wagner F, Seemann R, Marincola, et al. Fixed, fiber- reinforced resin bridges on four short implants in severely atrophic maxillae: 1-year results of a prospective cohort study. J Oral Maxfac Surg. 2018;76(6):1194–1199.
- Ewers R, Marincola M, Morgan V, et al. “All on three” - Kunststoffprothesen auf drei Implantaten. Zm 108/13, Juni 2018
- Görürgöz C Öztas B. Anatomic characteristics and dimensions of the nasopalatine canal: a radiographic study using cone-beam computed tomography. Folia Morphologica. 2020.
- Ewers R. Reduktion der Implantatzahl im Oberkiefer bei kurzen Implantaten. Implantatinsertion ins Foramen incisivum – erste Ergebnisse. Implantologie. 2018;26(4):415–425.
- Al-Amery S, Nambiar P, Jamaludin M, et al. Cone Beam Computed Tomography Assessment of the Maxillary Incisive Canal and Foramen: Considerations of Anatomical Variations When Placing Immediate Implants. PLoS One. 2015;10(2):e0117251.
- Friedrich RE, Laumann F, Zrnc T, et al. The Nasopalatine Canal in Adults on Cone Beam Computed Tomograms - A Clinical Study and Review of the Literature. In Vivo. 2015;2(4)9:467–486.
- Jayasinghe RM, Hettiarachchi PVKS, Fonseka MCN, et al. Morphometric analysis of nasopalatine foramen in Sri Lankan population using CBCT. Journal of Oral Biology and Craniofacial Research. 2020;10(2):238–240.
- Ewers R. On-Demand-Webinar: Möglichkeiten und Grenzen beim Einsatz von kurzen und ultrakurzen Implantaten. 2018.
- Leboucq H. Le canal nasopalatin chez l’homme. In: Arch Biol Paris. 1881;2:386–397.
- Allard RH, de Vries K, van der Kwast WA. Persisting bilateral nasopalatine ducts: a developmental anomaly. Oral Surg Oral Med Oral Pathol. 1982;53:24–26.
- Vollmer R, Vollmer M, Nimtschke U, et al. Bedeutung des Foramen incisivum bei Implantationen in der Prämaxilla. Implantologie Journal. 2018.
- Bell WH. Revascularization and bone healing after anterior maxillary osteotomy: a study using adult rhesus monkeys. J Oral Surg. 1969;27(4):249–255.
- Härle F, Ewers R. Die Hufeisenosteotomie mit Knochen- interposition zur Erhöhung des Oberkieferkammes - eine im Experiment steckengebliebene Operationsmethode. Dtsch Zahnärztl Z. 1980;35:105–107.
- Yerit KC, Posch M, Guserl U, et al. Rehabilitation of the Severely Atrophied Maxilla by Horseshoe Le Fort I Osteotomy (HLFO). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(60:683–692.
- Bodereau EF, Flores VY, Naldini P, et al. Clinical Evaluation of the Nasopalatine Canal in Implant-Prosthetic Treatment: A Pilot Study. Dent J. 2020;8(2):30.
- de Mello JS, Faot F, Correa G, et al. Success rate and complications associated with dental implants in the incisive canal region: a systematic review. Int J Oral Maxillofac Surg. 2017;46(12):1584–1591.
- Ewers R, Perpetuini P, Morgan V, et al. TRINIA™-Metal-free restorations. Implants 2017;1:2–7.
- Kern M, Att W, Fritzer E, et al. Survival and Complications of Single Dental Implants in the Edentulous Mandible Following Immediate or Delayed Loading: A Randomized Controlled Clinical Trial. J Dent Res. 2018;97(2):163–170.
- Asami M, Kanazawa, Lam TV, et al. Preliminary study of clinical outcomes for single implant-retained mandibular overdentures. Journal of Oral Science. 2020;62(1):98–102.
- Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–236.
- Ewers R. The incisal foramen as a means of insertion for one of three ultra-short implants to support a prosthesis for a severely atrophic maxilla - A short-term report. Heliyon. 2018;4(12):e01034.
- Ewers R. Pedicled Sandwich Osteotomy - surgical technique for vertical and horizontal alveolar bone deficiency. Vortrag auf dem International Bone Symposium in Implant Dentistry in San Francisco/USA am 30.3. 2017.
- Neugebauer J, Vizethum F, Berger C, et al. Update: Kurze, angulierte und durchmesserreduzierte Implantate – Praxisleitfaden: 11. Europäische Konsensuskonferenz (EuCC). BDIZ/EDI Konkret. 2016;20:88–90.
- Ravidà A, Wang IC, Barootchi S, et al. Meta-analysis of randomized clinical trials comparing clinical and patient-reported outcomes between extra-short (≤6 mm) and longer (≥10 mm) implants. J Clin Periodontol. 2019;46(1):118–142.
- Rameh S, Menhall A, Younes. Key factors influencing short implant success. Oral Maxillofac Surg. 2020;24(3):263–275.
- Lombardo G, Pighi J, Marincola M, et al. Cumulative Success Rate of Short and Ultrashort Implants Supporting Single Crowns in the Posterior Maxilla: A 3-Year Retrospective Study. Int J Dent. 2017;2017:8434281.
- Felice P, Checchi L, Barausse C, et al. Posterior jaws rehabilitated with partial prostheses supported by 4.0 x 4.0 mm or by longer implants: One-year post-loading results from a multicenter randomised controlled trial. Eur J Oral Implantol. 2016;9:35–45.
- Pohl V, Thoma DS, Sporniak-Tutak K, et al. Short dental implants (6 mm) versus long dental implants (11-15 mm) in combination with sinus floor elevation procedures: 3-year results from a multicenter, randomized, controlled clinical trial. Journal of Clinical Periodontology. 2017;44(4):438–445.
- Vazouras K, Barbisan de Souza A, Gholami H, et al. Effect of time in function on the predictability of short dental implants (≤6mm): a meta‐analysis. J of Oral Rehabilitation. 2020;47(3):403–415.
- Kern JS, Terheyden H, Wolfart S. Implantat-prothetische Versorgung des zahnlosen Oberkiefers. S3-Leitlinie. AWMF-Registernr. 083–010. .2017, Report No.: AWMF-Registernr. 083–010: AWMF.
- Seemann R, Marincola M, Seay D, et al. Preliminary Result of Fixed, Fiber-Reinforced Resin Bridges on Four 4- x 5- mm Ultrashort Implants in Compromised Bony Sites: A Pilot Study. J Oral Maxillofac Surg. 2015;73(4):630–640.
- Seemann R, Wagner F, Marincola M, et al. Fixed, Fiber- Reinforced Resin Bridges on 5.0-mm Implants in Severely Atrophic Mandibles: Up to 5 Years’ Follow-Up of a Prospec- tive Cohort Study. J Oral Maxillofac Surg. 2018;76(5):956–962.
- Ewers R, Perpetuini P, Seemann R, et al. Atrophic Maxillary Ridges. In: Morgan VH, editor. The Bicon Short Implant: A Thirty-Year Perspective. Chicago: Quintessence Publishing, 2017:199–213.
- Kern JS, Kern T, Wolfart S, et al. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016;27(2):174–195.
- Ewers R, Seemann R. TRINIA™ Trio – „all-on-three“ – metallfreie glasfaserverstärkte Kunststoffprothese auf drei ultrakurzen Bicon-Implantaten. Zahn Krone 3/17:11–17.
- Wolff J. Das Gesetz der Transformation der Knochen. Berlin: Verlag von August Hirschwald, 1892.
- Schlegel KA, Schmitt CH, Möst T. Implantate beim hochbetagten Patienten?! Fallserie hochbetagter Patienten Implantologie. 2020;28(2):157–166.
- Knöfler W, Barth T, Graul R, et al. Beobachtung von 10.000 Implantaten über 20 Jahre-eine retrospektive Studie. Einfluß von Implantatlänge, durchmesser und -typ auf die Überlebensrate. Implantologie. 2017;25($):413–421.