Volume : 4 | Issue : 1
Research
Modified quadrangular LeFort I osteotomy on a Crouzon Syndrome patient: A case report
Marcus Antônio Brêda Júnior,1 Davi Luiz Lage Cortez,2 Ricardo Viana Bessa-Nogueira,3 José Ricardo Mikami4
1DDS, MSc, Associate Professor, Oral and Maxillofacial Surgery, Dental School, Centro Universitário Tiradentes, Brazil
2Undergraduate – Dental School, Centro Universitário Tiradentes, Brazil
3DDS, MSc, PhD, Associate Professor, Oral and Maxillofacial Surgery, Dental School, Federal University of Alagoas, Brazil
4DDS, Specialist, Oral and Maxillofacial Surgery, Hospital das Clínicas, University of São Paulo, Brazil
Received: June 16, 2021 | Published: July 20, 2021
Abstract
Crouzon Syndrome is a genetically inherited condition presenting phenotypic variability, classified as discrete to severe, which affects the facial profile leading to psychosociological and functional disorders. Orthognathic surgery is a reliable treatment modality to correct the facial profile asymmetry and malocclusion in patients affected by this congenital syndrome. A female patient diagnosed with Crouzon Syndrome was referred to a surgeon for management of the craniofacial deformity. Eight millimeters of maxillary advancement was indicated to correct the skeletal dental deformity. During the surgery, a Quadrangular LeFort I was carried out with a modification in the traditional osteotomy design, a smooth ascendant curve was made at the pyriform aperture (5 mm below the infraorbital foramen), aiming to minimize the premature contact points and prevent a bony step-off due to the significant maxillary advancement. The reported modified Quadrangular LeFort I osteotomy was able to correct the patient’s midface hypoplasia, and no complications were reported during the postoperative follow-up.
Keywords: crouzon syndrome, craniofacial dysostosis, midface hypoplasia, lefort i osteotomy, orthognathic surgery
Introduction
Crouzon Syndrome (CS) was described as the most common among the craniosynostosis, that is, syndromes that lead to premature fusion of the cranial sutures,1 being surpassed by the most recently described Muenke syndrome. 2 It is a genetically inherited condition, carried on through dominant autosomal heritage, presenting phenotypic variability classified as discrete to severe.1,3 Diagnosis is obtained by clinical and radiographic examination, as the phenotypic evidence shows up by the first years of life. The patients affected by this syndrome may present significant facial deformities, such as brachycephaly, hypertelorism, proptosis, flattened forehead, beaked nose, and maxillary/midface hypoplasia. Cleft lip and/or palate, hearing loss, dental problems and strabismus are also described as very common in these patients, that clinical features can be compromising by leading to psychosociological and functional disorders.2
Orthognathic surgery may be performed to correct the facial profile and occlusion in patients affected by congenital syndromes, with a long-term stability of the dental and skeletal structures.4 (Nguyen et al., 2016). Moreover, it is a reliable treatment option, especially in the CS patients population, due to the need for a significant midface advancement.5
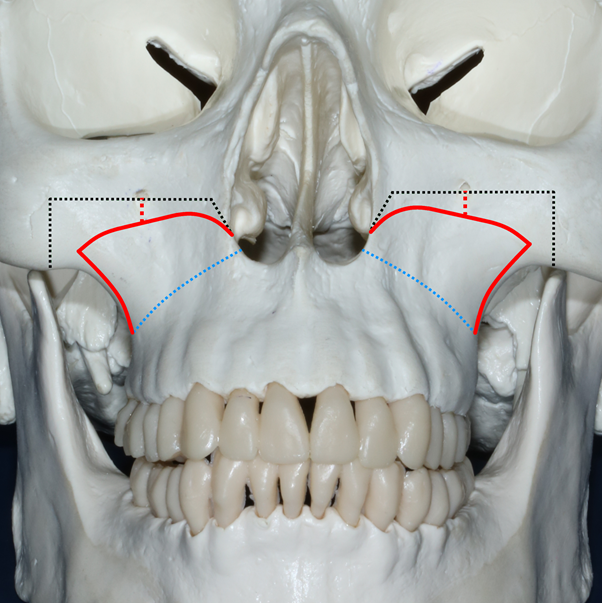
The current case report suggests, therefore, a modification in the design of the Quadrangular LeFort I osteotomy (QLF-I), preconized by Keller & Sather, 1990, aiming to minimize the risk of iatrogenic accidents by leaving a security margin to the infraorbital foramen. Moreover, this modification was done to avoid including a massive portion of the zygomatic bone and prevent a bony step-off due to the significant maxillary advancement needed in CS patients (severe midface hypoplasia).
Case report
A 25-years-old female patient affected by Crouzon Syndrome was referred to an oral and maxillofacial surgeon in order to conclude her orthosurgical treatment and reported a chief complaint of facial hypoplasia, the patient did not refer to any previous consultation in order to treat her complaints. At the exam, the patient reported persistent epilepsy episodes, and no additional systemic pathologies or drug allergies were reported. Facial photographs, radiographic analysis (panoramic and cephalometric radiographic), and the analysis of dental models were performed. A class III facial profile, with a significant maxillary anteroposterior deficiency, but with an adequate dental alignment was noted. At clinical examination, the following features were observed: hypertelorism, divergent strabismus and amaurosis (on the left eye), an inferior inclination of the nasal apex, obtuse nasolabial angle, lip incompetence, and a deficit on the paranasal and zygomatic regions.
Based on the clinical examination and cephalometric prediction tracings, a maxillary advancement of eight millimeters was planned to correct the retroposition of the maxilla. Moreover, the radiographic exam suggested that the patient had a narrow retropharyngeal space. Thus, aiming to prevent a worsening of the upper airway patency, no surgery was done in the mandible. Since the surgery was done via the brazilian public health system, (Sistema Único de Saúde - SUS) the Virtual Surgical Planning was not included in the budget, therefore, the surgery was planned in the traditional model.
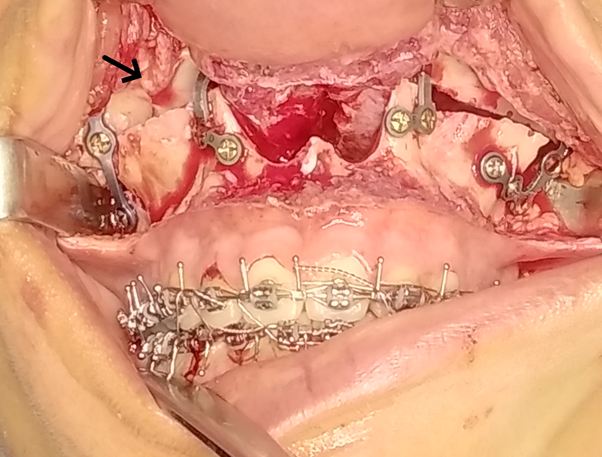
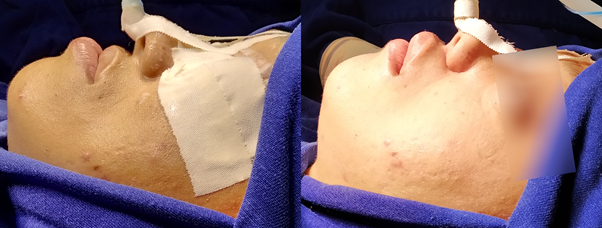
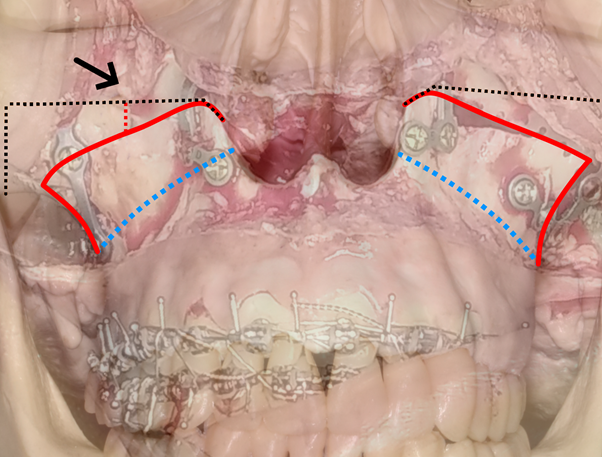
The patient was operated under general anesthesia and nasotracheal intubation. A standard maxillary vestibular incision, from the midline to first molar distal regions, was performed bilaterally followed by tissue dissection and subperiosteal elevation until exposure of the lower orbital edges and malar prominence with preservation of the infraorbital nerves. A QLF-I osteotomy was carried out with a modification in its design (Figure 1). The infraorbital foramen was used as a landmark, and the upper limit of the osteotomy was approximately 5 mm below it. The osteotomy was started with a reciprocating saw in the largest concavity of the piriform recess, similar to the standard QLF-I osteotomy, but done in an ascendent slight curvature fashion. From this point, the osteotomy runs inferiorly to the infraorbital foramen and, following the curvature of the ridge, passed through with a safety margin of 5 mm below the infraorbital foramen until it approximated the malar prominence. Without penetrating the malar prominence, the orientation of the saw was modified, now vertically to caudal, ending the osteotomy in the lateral pillar of the maxilla approximately where a conventional Le Fort I osteotomy would end. Chisels were used to complement the osteotomies of the lateral wall of the nose and nasal septum and with a curved chisel, the pterygoid-palatal disjunction was performed. As in the conventional Le Fort I osteotomy, the maxilla was mobilized in the caudal direction with a digital maneuver to verify its mobility. The use of Rowe's clamps for complete maxillary repositioning required exceptional care, to avoid an undesirable fracture of the anterior wall of the maxillary sinus, contained in the maxillary block. The maxilla was positioned according to the prefabricated acrylic resin interocclusal splint, and the maxillomandibular fixation (MMF) with steel wire was done. Then, osseous interferences were removed, and the maxilla was initially fixated using two “L” plates and eight screws on the nasomaxillary buttresses. After the release of MMF, the occlusion was checked, and an adequate intercuspation was achieved, an additional two “L” plates and eight screws were used on the zygomaticomaxillary buttresses (Figure 2 & 3). The total amount of anterior maxillary advancement was eight millimeters, and the inferior reposition was two millimeters, adequately resolving the prior midface hypoplasia (Figure 4).
|
Figure 3 Overlap of figures 1 and 2. Illustration made on the dry skull of the planned osteotomy redesign on the transoperative photography. |
At 24 months of postoperative follow-up, a satisfactory and stable correction of the patient’s midface hypoplasia and occlusion was observed, and no complications were reported.
Discussion
The current case report sought to report the use of a modified QLF-I to treat severe maxillary hypoplasia in a female CS patient. Maxillary hypoplasia is commonly seen in CS patients,1,2,4 which usually demands a significant maxillary advancement to correct it. Usually, a LeFort I osteotomy is advocated to correct maxillary hypoplasia.6 However, depending on the patient’s aesthetic needs, a QLF-I osteotomy, which is designed with a vertical extension (including the infraorbital foramen), could be accurately indicated to resolve the severe midface hypoplasia.5,7 However, due to the risk of injury to the infraorbital nerve, the authors of the current technical note suggest a modification (a safe margin of 5mm below infraorbital foramen). Moreover, the redesign of the osteotomy permitted an adequate improvement on midface projection without needing to include a massive portion of the zygomatic body, granting effectiveness within minimal collateral damage.
Described by Obwegeser in 1969, LeFort I osteotomy has been carried out under some modifications to attend patients’ needs in different ways. Kaminishi and associates8 reported a modification which aimed to avoid the thin maxillary bone to achieve a more solid fixation by including the zygomatic body, and the cut ran from piriform aperture laterally and slightly superiorly reaching 5 mm from the inferior portion of the zygomatic process of the maxilla. Bennett & Wolford9 on the other hand, carried out a step LeFort I osteotomy, allowing a downslide of the maxillary bone and that the operator could utilize bone grafts in a more convenient position, but, no significant modification on the height of the osteotomy is reported.
Abubaker & Sotereanos,10 evaluated 38 patients who had undergone “zygomatic-maxillary modified LeFort I osteotomy” which resembled the modification suggested by Kaminishi, also including zygoma and stopping 7-10 mm before the anterior-inferior border of the zygomatic arch, on this study, the authors warned about the risk of some hassles concerning this modification, such as inadvertent additional fractures during the down fracture, because of the inclusion of a portion of the zygomatic bone alongside the maxilla; the technical difficulty of the procedure; and if the patient needs a significant anterior reposition of the midface no bone contact on the zygomatic region was observed.
Nørholt and colleagues,11 presented a modification which goal was to approach the infraorbital rim (including the zygomatic bone body), deviating laterally the infraorbital foramen and ascending the osteotomy until 3-4 mm from the infraorbital margin. The anterior mentioned authors suggested that this technique should be classified as a modified LeFort II osteotomy, as the proposed osteotomy approaches closely to the infraorbital rim.
After a careful literature review, the authors of the current technical note could observe that there are abundant reports of modification in LeFort I osteotomy design.8–11 However, few or none of the reports presented the use of a modification on the osteotomy design to resolve midface hypoplasia on a CS patient. Therefore, to the best of our knowledge, this is the first technical note that addressed this clinical issue in a specific patient population.
In the same context, Nørholt and colleagues,11 initially advocated that LeFort III osteotomy would be the standard osteotomy for the treatment of craniofacial syndromes patients. Meanwhile, Nakajima and associates7 suggested that LeFort I osteotomy should be the preferable procedure used to treat these deformities, because of its technical plainness, low complication rate, and broad applicability, permitting a great variety of modifications to attend the patient’s necessity and minimizing the surgical traumas caused by more complicated surgeries.7,12 Moreover, the anterior mentioned authors reported that LeFort III is a highly invasive approach and postoperative complications are frequently reported.
In the first view, our osteotomy design is somewhat similar to QLF-I carried out by Keller & Sather. However, our modification sought to minimize its invasiveness leaving a safety margin (five millimeters) from the infraorbital foramen to avoid injury to the infraorbital nerves. Due to the fact that the current osteotomy presents a slight ascendent curvature, it prevents a bony step-off due to the tremendous maxillary advancement needed in CS patients. The surgeon was able to treat significant midface hypoplasia using the current modified QLF-I osteotomy, which is commonly seen on patients affected by CS. Moreover, the surgery was carried out with fewer technical difficulties, and no bone grafts were used. In the same context, the study of Stork and associates suggest that QLF-I is a safe, stable, and surgically predictable osteotomy with or without the use of bone grafts.13
Despite the exceptional result reported in this technical note, our study has some limitations, and our result should be understood in the context of clinical practice. The first limitation is that the current report is not a case series or a clinical trial. Future studies should compare the result of different LeFort osteotomy designs for the treatment of CS patients. Second, our modification sought to minimize the risk of nerve injury suggesting an alternative osteotomy design, however, due to this technical note comprise a single patient, more studies of nerve injury following the use of this osteotomy are advised. However, CS is a rare disease, and a case series will be a challenging task. Third, our surgical approach did not address the correction of the alterations on the orbit. In daily practice, the current authors observed that the chief complaint of the craniofacial patients resumes to the facial middle third, and most of them seem to be satisfied with the single correction of the middle third and the dental occlusion. The same was reported by the current patient, and all surgical aspects were discussed before the surgery.
Acknowledgements
None.
Funding
None.
Conflicts of Interest
The authors have no conflict of interest to disclose.
References
- Kalanjiam V, Manoharan GVMG. Crouzon Syndrome - a rare case report. Int J Health Sci (Qassim). 2017;11(4):74–75.
- Conrady CD, Patel BC. Crouzon Syndrome. Treasure Island, Florida: StatPearls Publishing; 2019.
- Al-namnam NM, Hariri F, Thong MK, et al. Crouzon Syndrome: Genetic and intervention review. J Oral Biol Craniofac Res. 2019;9(1):37–39.
- Nguyen PD, Caro MC, Smith DM, et al. Long-term orthognathic surgical outcomes in Treacher Collins patients. JPRAS. 2016;69(3):402–408.
- Keller EE, Sather AH. Quadrangular Le Fort I osteotomy: surgical technique and review of 54 patients. J Oral Maxillofac Surg. 1990;48(1):2–13.
- Obwegeser HL. Surgical correction of small or retrodisplaced maxillae. The "dish-face" deformity. Plast Reconstr Surg. 1969;43(4):351–365.
- Nakajima Y, Nakano H, Sumida T, et al. High Le Fort I osteotomy for correction of mid-face deformity in Crouzon syndrome. Congenit Anom (Kyoto). 2016;56(5):240–242.
- Kaminishi RM, Davis WH, Hochwald DA, et al. Improved maxillary stability with modified Lefort I technique. J Oral Maxillofac Surg. 1983;41(3):203–205.
- Bennett MA, Wolford LM. The maxillary step osteotomy and Steinmann pin stabilization. J Oral Maxillofac Surg. 1985;43(4):307–311.
- Abubaker AO, Sotereanos GC. Modified Le Fort I (maxillary-zygomatic) osteotomy: rationale, basis, and surgical technique. J Oral Maxillofac Surg. 1991;49(10):1089–1097.
- Nørholt SE, Sindet-Pedersen S, Jensen J. An extended Le Fort I osteotomy for correction of midface hypoplasia: a modified technique and results in 35 patients. J Oral Maxillofac Surg. 1996;54(11):1297–1306.
- Avelar RL, de Souza MSM, Soares ECS, et al. Use positional screws for Le Fort I osteotomy fixation: technical note. Oral Maxillofac Surg. 2017;21(3):347–349.
- Stork JT, Kim RH, Regennitter FJ, et al. Maxillary quadrangular Le Fort I osteotomy: long-term skeletal stability and clinical outcome. Int J Oral Maxillofac Surg. 2013;42(12):1533–1546.