Volume : 5 | Issue : 1
Case Report
A Quantitative Analysis Of PRF As The Sole Treatment Modality In Aiding Bony Regeneration In Cystic Cavities: A Case Report
Karan Padha,1 I D Roy,2 Yuvraj Issar,3 Anup Singh4
12075 Fd Hospital, Bhuj, India
2,3,4Department of Oral & Maxillofacial Surgery, AFMC Pune, India
Received: December 25, 2022 | Published: December 30, 2022
Abstract
Background: Spontaneous regeneration of bony defects has long been considered the gold standard after the enucleation of jaw cysts. Horowitz et al used a combination of Kiel bone in combination with autologous aspirated bone marrow as a grafting material in cystic cavities while Mitchell evaluated the efficacy of collagen matrix. Over the years, various substitutes like DFDBA, xenografts, and synthetic grafts have been tried without offering significant benefits over spontaneous regeneration. However, PRF as a sole treatment modality with its angiotrophic, hemostatic, and osseous conductive properties and its quantitative role in aiding bony regeneration has not been explored.
Case Presentation: We present two cases that underwent enucleation and peripheral ostectomy followed by A-PRF placement to aid bony regeneration. Preop and 6th-month postop OPG were quantitatively analyzed for a reduction in the size of the cystic cavity.
Conclusion: The case series aims to understand the role of PRF in aiding bony regeneration using digital analysis of the cystic cavities and assessing the actual statistical reduction achieved by using this treatment modality.
Keywords: PRF, Primary Closure, Dentigerous Cyst, Enucleation
Abbrevations
PRF, platelet rich fibrin; DFDBA, demineralized freeze dried bone allograft; OPG, orthopantomagram; PDGF, platelet derived growth factor; FGF, fibroblast growth factor; VEGF, vascular endothelial growth factor; BMP, bone morphogenetic protein; TGF, transforming growth factor
Background
Spontaneous regeneration is the gold standard for bony fill in cystic cavities as advocated in the literature. PRF as an adjunct to bony healing has never been quantitatively explored in literature, especially in larger cystic defects. In this case report series, we present two cases of dentigerous cysts of varying dimensions managed by enucleation and peripheral ostectomy followed by A-PRF placement. We digitally analyze its performance in aiding bony regeneration in a bid to substantiate its claim as a viable alternative for cystic defects.
Case Presentation
Case Report 1
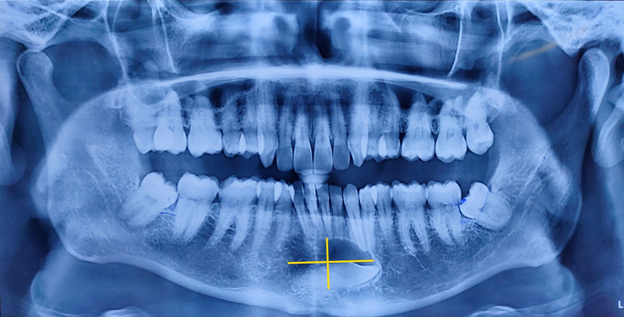
A 22-year-old man reported to the Division of Oral and Maxillofacial Surgery after incidentally discovering a cyst during the preoperative OPG examination for third molar extraction. On intraoral examination, 43 were found to be clinically missing. An aspiration biopsy was done yielding straw-colored fluid with a histopathologi-cal diagnosis of a benign cystic lesion. A pre-op OPG Figure 1 was done revealing an impacted 43 in relation to a cystic cavity. Pre-op CBCT was done revealing a cystic cavity measuring 10.41 x 16.73 x 7.45 mm with buc-cal cortical thinning and approximation to the mental foramen. Enucleation with peripheral ostectomy and extraction of the impacted canine was carried out. A-PRF was harvested from the patient with the set parame-ters: 1500 rpm, 208 g centrifugation force, and 14 min centrifugation time. The extracted A-PRF was packed into the cystic cavity and closure was completed. Postoperative healing was uneventful with no neurosensory deficit. The patient maintained follow-up for a 6-month period Figure 2.
Case Report 2
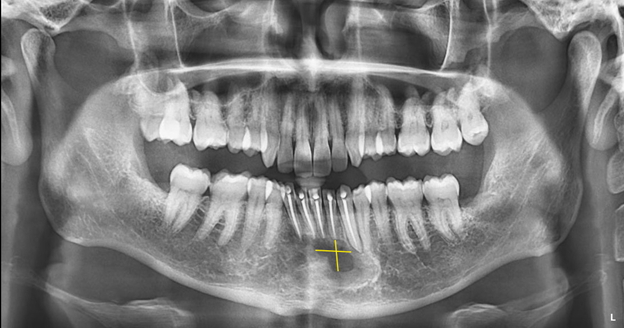
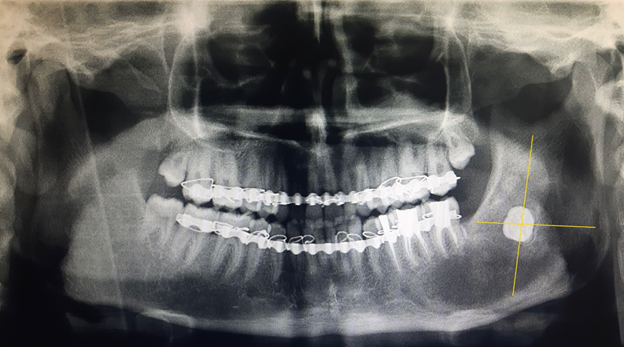
An 18-year-old adolescent boy was reported to the Division of Oral and Maxillofacial Surgery with a chief complaint of swelling over the lower left side of his face. Aspiration biopsy established a histopathologic diagnosis of a benign cystic lesion. An OPG Figure 3 was done revealing well-defined uni-locular radiolucency extending from the mandibular body to the sigmoid notch. 38 was found to be impacted and circumferentially enveloped by the cystic lesion. A two-stage treatment plan was formulated with decompression of the cystic lesion carried out in the first stage followed by enucleation and peripheral ostectomy with PRF placement in the second stage. A- PRF was harvested from the patient with the set parameters: 1500 rpm, 208 g centrifugation force, and 14 min centrifugation time Figure 4. The extracted A-PRF was packed into the cystic cavity and closure was completed. Postoperative healing was uneventful with no neurosensory deficit. The patient maintained follow-up for a 6-month period Figure 5.
Discussion
Spontaneous regeneration has long been considered the gold standard following enucleation of jaw cysts however, there is still no clear consensus regarding bony healing and the role of substitutes in larger cystic defects. Horowitz et al used a combination of Kiel bone in combination with autologous aspirated bone marrow as a grafting material in 20 patients with medium and large-size defects of the jaws and reported a failure rate of 20% involving one medium-sized and 3 large cysts.1 Mitchell evaluated the efficacy of collagen matrix in 50 patients and reported that collagen delayed the healing period which was especially more pronounced in the early phase of bone healing and concluded that collagen being osteoinductive, bony healing can only take place after its degradation.2 A variety of substitutes like DFDBA, xenografts, and synthetic grafts have been explored however there is no clinical data suggesting a reduction in the risk of infection during primary wound healing.3 PRF as the sole grafting alternative has started finding application in radicular cystic cases as well as for maxillary sinus augmentation.4-6 However, it is quantitative role in aiding bony regeneration in terms of actual statistical reduction in the cystic defect, especially in larger cystic cavities has not been explored. The case for PRF rests on its angiotrophic, hemostatic, and osseous conductive properties due to the presence of fibrin in PRF which acts as a recognized support matrix for bone morphogenetic proteins (BMP). The progressive release of cytokines is a common feature of in vivo natural fibrin clots and likely of PRF. The platelet cytokines namely TGF Beta 1 (Fibrosis agent), PDGF (Stimulant of mesenchymatous lineages), and IGF ( Cell protective agent) help in inducing fibrin matrix and cicatricial matrix remodeling thus yielding a synergistic effect on the healing process. Furthermore, through angiogenesis soluble factors such as fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and platelet-derived growth factor (PDGF), PRF acts as fibrin-based biomaterial favoring micro vascularization and accelerating healing.7 We evaluated this hypothesis by Choukran and quantitatively studied its effect on accelerating bony healing. A-PRF was extracted using set parameters of 1500 rpm, 208 g centrifugal force, and a time duration of 14 minutes. After discarding the topmost platelet poor plasma layer and the bottom RBC layer, the A-PRF was condensed into the cystic cavity.
According to Chiapasco et al, 2000 and Ihan Hren and Miljavec, 2008 spontaneous bony healing of large mandible bone defects recovered bone density by 7%, 27% and 46% after 2, 6 and 12 months respec-tively. However, in smaller defects measuring 2 x 3 cm in diameter, a final bone density of 97% in relation to normal surrounding bone was observed after 12 months.8 Chiapasco et al further stated that spontaneous bony regeneration of cysts larger than 4 cm showed a mean reduction in size of 12.3%, 43.5% and 81.3% after 6, 12 and 24 months and an increase of bone density of 37.0%, 48.2% and 91.0% after 6, 12 and 24 months on computed analysis of panoramic radiographs.9 We evaluated these observations and compared it to healing characteristics following A-PRF placement. The pre and postoperative OPG’s were digitally analyzed and the data converted into pixels for quantitative analysis. In Case 1, the preoperative number of pixels measured for the cystic defect were 104047.78 Figure 1. At 6th month postoperative follow up, the number of pixels meas-ured for the cystic defect were 13515.64 Figure 2. A reduction in size and bony healing of 87.02 % was achieved. In Case 2, the preoperative number of pixels measured for the cystic defect were 286872 Figure 3. At 6th month postoperative follow up, the number of pixels measured for the cystic defect were 125137.66 Figure 4 & 5. Thus equating to a 56 % reduction in size and concomitant bony healing. In both cases the mean reduc-tion in size (87.02% and 56%) far exceeded that quoted in literature (12.3%) at the 6th month postoperative period.
Conclusion
The study conducted reinforces the claim that A-PRF when used as a sole treatment modality does significantly help in postoperative bony healing in cystic cavities as compared to spontaneous bony regeneration. It marks an exciting and accessible treatment modality not just in small radicular cystic cases but even in larger cystic defects like dentigerous cyst, with the potential to cause a paradigm shift in how we think of bony healing in cystic cavities.
Acknowledgements
None.
Conflicts of Interest
None.
References
- Horowitz I, Bodner L. Use of xenograft bone with aspirated bone marrow for treatment of cystic defect of the jaws. Head Neck. 1989;11(6):516‒523.
- Mitchell R. An evaluation of bone healing in cavities in the jaws implanted with a collagen matrix. Br J Oral Maxillofac Surg. 1992 ;30(3):180‒182.
- Ettl T, Gosau M, Sader R, Reichert TE. Jaw cysts - filling or no filling after enucleation? A review. J Craniomaxillofac Surg. 2012 Sep;40(6):485‒493.
- Dhote VS, Thosar NR, Baliga SM, Dharnadhikari P, Bhatiya P, et al. Surgical Management of Large Radicular Cyst Associated with Mandibular Deciduous Molar Using Platelet-rich Fibrin Augmentation: A Rare Case Report. Contemp Clin Dent. 2017 Oct-Dec;8(4):647‒649.
- Zhao JH, Tsai CH, Chang YC. Clinical application of platelet-rich fibrin as the sole grafting material in maxillary sinus augmentation. J Formos Med Assoc. 2015 Aug;114(8):779‒780.
- Mitrea Mihaela, Rusu Anca, Călin, Dorelia. The Management Of Periapical Maxillary Cyst By Using The A-Prf (Platelet Rich Advanced Fibrin): A Case Report. Romanian Journal of Oral Rehabilitation. 2015;7(2):12‒19.
- Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e56‒60.
- Ihan Hren N, Miljavec M. Spontaneous bone healing of the large bone defects in the mandible. Int J Oral Maxillofac Surg. 2008 Dec;37(12):1111‒1116.
- Chiapasco Matteo, Rossi Alessandro, Motta Jones Jason, Crescentini Michele. Spontaneous bone regeneration after enucleation of large mandibular cysts: A radiographic computed analysis of 27 consecutive cases. Journal of oral and maxillofacial surgery: Official journal of the American Association of Oral and Maxillofacial Surgeons. 2000;58(9): 942‒948.