Volume : 6 | Issue : 1
Clinical Study
Outcome of Vital Pulp Therapy Using Bioceramic Materials: A Retrospective Clinical Study
Su-Min Lee*, Nhan James H. Ngo, Ya-Hsin Yu, Bekir Karabucak
Department of Endodontics, School of Dental Medicine, University of Pennsylvania, 240 S. 40th Street, Philadelphia, PA 19104-6030, USA
Received: February 16, 2023 | Published: March 02, 2023
Abstract
Purposes: The aim of this retrospective study was to investigate the clinical and radiographic outcome of vital pulp therapy (VPT) procedures, including indirect pulp capping (IPC), direct pulp capping (DPC), a partial pulpotomy (PP), and full pulpotomy (FP) using EndoSequence® Bioceramic Fast-Set putty (BC-RRMFS) in permanent teeth.
Materials and methods: VPT cases performed in the postgraduate endodontic clinic at the University of Pennsylvania were collected based on strict criteria. The treatment outcome was assessed clinically and radiographically with a minimum 6-month and a maximum 36-month follow-up.
Results: In cases from 66 patients (mean age, 18 years) were evaluated. Case distribution was as follows: IPC (38%), DPC (32.4%), PP (11.3%), and FP (18.3%). Molars were dominant in all treatment groups except the PP group. The majority of treated cases were pre-operatively diagnosed as reversible pulpitis (80.3%). Carious pulp exposures were the main etiology (85.9%). Pulp exposure was mostly on the occlusal surface (77.5%). The success rates of IPC and FP were 100% at all assessment time points. The success rates of DPC and PP at 6 to 11 months were 100%, and at the last follow-up appointments, both were 75%. Twelve teeth developed a failure that required a root canal treatment. The patient’s age, gender, pulpal diagnosis, pre-operative percussion tenderness, and, pulp exposure type/location were not statistically related to the success of VPT (p > 0.05).
Conclusions: The findings of this study suggest that VPT with BC-RRMFS can be suitable for the management of carious and traumatic pulp exposure in permanent teeth.
Keywords: vital pulp therapy, calcium silicate-based cement, BC-RRMFS, reversible pulpitis, success rate
Introduction
The established treatment goals in endodontics are to prevent and/or eliminate apical periodontitis. Prevention of the disease can be achieved by preserving the vitality of the dental pulp. Maintaining pulp vitality has numerous advantages, including allowing for continued root development, relieving symptoms, and promoting pulp tissue healing via tertiary dentin deposition.1 Preserving pulp vitality can be accomplished through vital pulp therapy (VPT), including pulp capping and pulpotomy.
In the past, materials such as eugenol2 or calcium hydroxide3–7 have been selected as the materials of choice for vital pulp therapy (VPT). However, the studies reported a range of clinical outcomes, resulting in the search for a superior class of materials with more consistent results. A class of hydraulic bioactive materials known as calcium silicate-based cement was developed in the endodontic field. Mineral Trioxide Aggregate (MTA) is the one material belonging to this family that has shown promising results in VPT.8 However, MTA is also difficult to handle and can cause tooth discoloration.9 EndoSequence® Bioceramic Fast-Set (BC-RRMFS) Putty (Brasseler, Savannah, GA) has been introduced and is available for use as an alternative to MTA providing easy handling and color stability. BC-RRMFS has been widely used in VPT and was shown to have a comparable outcome with MTA. However, the reports lacked information regarding the reasons for and the timing of the failure to use this specific material.
To our knowledge, there is no clinical study to evaluate the outcome of VPT using BC-RRMFS. Therefore, the purpose of this study was to investigate the clinical and radiographic success rates of VPT, including indirect pulp capping (IPC), direct pulp capping (DPC), a partial pulpotomy (PP), and full pulpotomy (FP) treated with BC-RRMFS in permanent teeth. Furthermore, the failure timeline and reasons for VPT were demonstrated.
Material and methods
The study protocol was approved by the Institutional Review Board (IRB) Committee at the University of Pennsylvania (IRB Protocol #843061). Patients who received VPT in permanent teeth at the postgraduate Endodontic Clinic, School of Dental Medicine, the University of Pennsylvania between July 1, 2015 and June 30, 2019 were included in this investigation. Patient charts whose treatment includes VPT were retrieved via an electronic search using axiUm software (Exan, Henry Schein Inc, Melville, NY). Data were further sorted and only cases treated with BC-RRMFS were included.
Case selection
Case selection was based on the following inclusion and exclusion criteria:
Inclusion criteria:
- No systemic diseases and no history of antibiotics and analgesic use.
- The patient has no history of spontaneous and/or radiating pain preoperatively.
- Vital pulp therapy cases identified as IPC, DPC, PP or FP.
- The tooth responds to pulp sensibility testing (cold and/or electric pulp test) preoperatively.
- The tooth responds within normal limits or has slight tenderness with percussion.
- The tooth is in a restorable condition.
- The presence of bleeding from the exposed pulp.
- Probing depths less than 5 mm.
Exclusion criteria:
- Cases presenting with a preoperative periapical lesion on periapical radiograph examination.
- Cases presenting with a lingering response to thermal stimuli.
- Presence of sinus tract or intraoral/extraoral swelling.
- Evidence of pulp necrosis/ Cases not responding to sensibility testing indicated nonvital pulps.
- Probing depths equal to or more than 5mm.
- Non-restorable teeth.
- Non-controlled bleeding during the
- Follow-up period less than six months.
Collected cases were reviewed to analyze preoperative information. Preoperative information included the tooth number, clinical signs and symptoms, and radiographic interpretation of the affected tooth.
Vital pulp therapy protocols
All cases treated had adequate anesthesia and rubber dam isolation, and all treatments were performed under a microscope (OPMI Pico; Carl Zeiss, Oberkochen, Germany). High-speed round or diamond bur was used to reveal sound dentin or until pulp exposure occurred during caries excavation. If no pulp was exposed, an IPC was performed. The site was rinsed with 3% sodium hypochlorite (NaOCl), followed by saline irrigation. 2 to 3 mm of BC-RRMFS was placed directly over the pulp and surrounding sound dentin and dabbed with a moist cotton pellet to facilitate setting. Upon setting, a liner (EndoSequence Bioceramic Liner; Brasseler, or Fuji IX; GC, Alsip, IL) was placed covering BC-RRMFS and surrounding dentin and followed by a permanent composite resin restoration. A DPC was indicated if pulp was exposed due to overzealous caries excavation through sound dentin. Hemostasis was achieved by placing a 3% NaOCl-soaked or saline-soaked cotton pellet over the exposure site. Hemostasis and the condition of the pulp and surrounding sound dentin were inspected under high magnification and then BC-RRMFS was placed on the exposure site including the surrounding sound dentin.
If the pulp exposure was due to caries excavation whereby caries extended into the pulp chamber, the remaining caries were removed to reveal sound dentin. Moreover, 3 mm of pulp tissue was removed with a new diamond bur. In case of complicated crown fracture, the inflamed superficial pulp tissue was removed with a sterile diamond bur. If hemostasis was reached within 5-10 minutes, then a partial pulpotomy procedure was completed by placing 3 mm of BC-RRMFS into the pulp chamber, followed by coverage with a liner and permanent resin restoration. When hemostasis could not be achieved, a full pulpotomy was performed. The entire coronal pulp was removed with a high-speed diamond bur and hemostasis was obtained with placing a 3% NaOCl-soaked cotton pellet. 3 mm of BC-RRMFS was placed along the entire pulp chamber floor, followed by a liner and permanent resin restoration.
Follow-up and outcome measures
The most recent date (month) was noted as the follow-up range for the patient. At follow-up appointments, the following standardized steps occurred:
- The patient was asked to update his/her medical history and report any changes.
- The patient was asked to report any symptoms or discomfort associated with the treated tooth.
- Radiographs (periapical and bitewings) were taken.
- A thorough clinical assessment of the treated tooth was completed, including a cold test, electric pulp test (EPT), percussion, palpation, and the presence or absence of swelling or sinus tract development.
- Documentation of any clinical changes to the tooth, including discoloration, presence or absence of a permanent restoration, marginal deficiencies, or fractures.
After gathering this information, cases were analyzed in terms of success/failure based on clinical criteria and radiographic evaluation according to the PAI index.10 Two calibrated endodontists (S.L, N.N) analyzed the radiographs. The case was deemed successful if upon follow-up or noted in the patient chart, the tooth was still present in the mouth, symptoms resolved, there was a normal response to thermal stimuli, and there was an absence of any signs of infection. Furthermore, dentin bridge formation and root maturation in immature teeth continued were also investigated. The initial VPT was deemed a failure if additional procedures were performed due to persistent/developing symptoms or signs of pulp necrosis or apical periodontitis upon follow-up. The reasons and timing for all failures were noted and further analyzed.
Statistical analysis
Statistical analysis of the data was performed using IBM SPSS Statistics Version 23 (IBM Corp, Armonk, NY). The distribution of clinical features was analyzed with Chi-square analysis and t-test. The Kaplan-Meier method was used to analyze the cumulative survival rate of VPT and was followed by log-rank tests to compare groups. The Cox proportional hazards model was used to investigate the predictive factors and estimate the hazard ratios with 95% confidence intervals (CIs). Statistical significance was set at 0.05 level.
Results
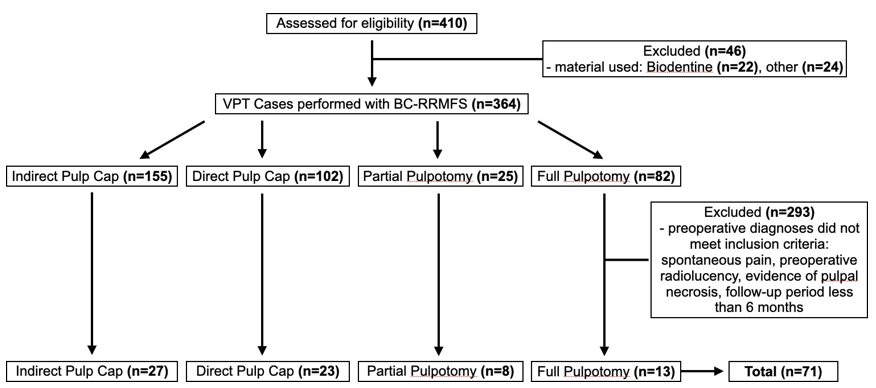
In total, 410 permanent teeth treated with VPT were collected from July 2015 to June 2019. A total of 71 teeth from 66 patients fulfilled the inclusion and exclusion criteria (Figure 1). The demographics and clinical characteristics of the study subjects in each treatment group are summarized in Table 1. Of the 71 teeth collected, 27 cases (38%) were treated by IPC, 23 cases (32.4%) by DPC, 8 cases (11.3%) by PP, and 13 cases (18.3%) by FP. The mean age was 18.06 years (range, 7-68 years), and 41 (58%) were male patients. Molars were dominant in the most of treatment groups except PP group. Most cases were pre-operatively diagnosed as reversible pulpitis (57 cases [80.3%]) and had negative responses from pre-operative percussion tests (63 cases [88.7%]). Carious pulp exposures were the main reason for treatment (61 cases [85.9%]), followed by traumatic injuries (10 cases [14.1%]). Among treatment groups, only the PP group has an equal number of pulp exposures from the carious lesion and traumatic injury. The location of pulp exposure was mostly on the occlusal surface (55 cases [77.5%]). There were no significant differences in age, sex, tooth type, diagnosis, or pulp exposure location among the four groups.
|
Total |
IPC |
DPC |
PP |
FP |
|
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
p value |
|
No. of cases/teeth |
71 (100) |
27(38) |
23 (32.4) |
8 (11.3) |
13 (18.3) |
|
Age (years±SD) |
18.06±14.22 |
26.48±19.21 |
15.39±6.91 |
10.13±2.75 |
10.15±2.23 |
0.31 |
Sex |
0.31 |
|||||
Male |
41 (57.7) |
16 (59.3) |
10 (43.5) |
6 (75) |
9 (69.2) |
|
Female |
30 (42.3) |
11 (40.7) |
13 (56.5) |
2(25) |
4 (30.8) |
|
Tooth type |
0.01 |
|||||
Anterior |
10 (14.8) |
4 (14.8) |
0 (0) |
4 (50) |
2 (15.4) |
|
Premolar |
3 (4.2) |
2 (7.4) |
0 (0) |
1 (12.5) |
0 (0) |
|
Molar |
58 (81.7) |
21 (77.8) |
23 (100) |
3 (37.5) |
11 (84.6) |
|
Pulp status/clinical diagnosis |
0.43 |
|||||
Normal Pulp |
14 (19.7) |
8 (29.6) |
3 (13) |
1 (12.5) |
2 (15.4) |
|
Reversible pulpitis |
57 (80.3) |
19 (70.4) |
20 (87) |
7 (87.5) |
11 (84.6) |
|
Pre-operative percussion test |
0.001 |
|||||
Negative response |
63 (88.7) |
26 (96.3) |
23 (100) |
6 (75) |
8 (61.5) |
|
Positive response |
8 (11.3) |
1 (3.7) |
0 (0) |
2 (25) |
5 (38.5) |
|
Pulp exposure type |
0.004 |
|||||
Caries |
61 (85.9) |
24 (88.9) |
23 (100) |
4 (50) |
10 (76.9) |
|
Trauma |
10 (14.1) |
3 (11.1) |
0 (0) |
4 (50) |
3 (23.1) |
|
Pulp exposure location |
0.4 |
|||||
Occlusal |
55 (77.5) |
19 (70.4) |
20 (87) |
7 (87.5) |
9 (69.2) |
|
Interproximal |
16 (22.5) |
8 (29.6) |
3 (13) |
1 (12.5) |
4 (30.8) |
|
Table 1 Patient Demographics and Analysis of Baseline Tooth Characteristics
IPC, indirect pulp capping; DPC, direct pulp capping; PP, partial pulpotomy; FP, full pulpotomy
Success rates of VPT
The follow-up period varied from six months to 36 months, and the median time of follow-up was 12 months. In cases with multiple follow-ups, the latest examination results were included. The success rates of IPC and FP were 100% at all assessment time points (6 to 22 months for IPC, 6 to 26 months for FP) (Table 2). The success rates of DPC and PP at 6 to 11 months were 100%, and at the last follow-up appointments (24 months for DPC and 18 months for PP) both were 75%. The examples of cases considered successes and failures are shown in (Figure 2 and 3). Furthermore, the Kaplan-Meier plots illustrate cumulative survival for each VPT (Figure 4). The plot indicated that the high survival rate of the IPC group could be maintained over 24 months. However, failed cases from the DPC group could be detected after 15 months and over 75% of the DPC group could maintain pulpal survival over 36 months (Figure 4A). While failed cases from the PP group could be observed after 12 months, the high survival rate of the FP group could be steady over 24 months (Figure 4B).
|
IPC (n=27) |
DPC (n=23) |
PP (n=8) |
FP (n=13) |
|||||||||||
|
6 to 11 months |
12 to 17 months |
≥18 months |
6 to 11 months |
12 to 17 months |
18 to 23 months |
≥ 24 months |
6 to 11 months |
12 to 17 months |
≥18 months |
6 to 11 months |
12 to 17 months |
18 to 23 months |
≥ 24 months |
|
Follow-up |
14 |
11 |
2 |
6 |
9 |
5 |
3 |
4 |
3 |
1 |
5 |
5 |
1 |
2 |
|
Failed |
0 |
0 |
0 |
0 |
1 |
1 |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
|
Cumulative Proportion Surviving |
100% |
100% |
100% |
100% |
90% |
75% |
75% |
100% |
75% |
75% |
100% |
100% |
100% |
100% |
|
Table 2 The Success Rates in the Follow-up Periods
Analysis of cases with unfavorable outcomes
Three teeth developed failure that required further intervention (Table 3). Two returned cases after DPC opted for RCT because of spontaneous pain. After clinical and radiographic examinations, the diagnosis for these teeth was symptomatic irreversible pulpitis with symptomatic apical periodontitis. In addition, one patient received an RCT after PP as a tooth was diagnosed with pulp necrosis at the 12- 12-month low-up. Among failed three cases, only one tooth was diagnosed with symptomatic apical periodontitis preoperatively and progressed as pulp necrosis at the one-year follow-up visit. This tooth with proximal caries received PP and a direct composite restoration, and the margins were well maintained.
Case no. |
Sex/ Age(y) |
Tooth no. |
Preoperative Pulpal diagnosis |
Preoperative Periapical diagnosis |
Pulp Exposure Location |
Pulp Exposure Location |
Observations of failed cases |
|---|---|---|---|---|---|---|---|
DPC #3 |
F/24 |
15 |
Reversible pulpitis |
Normal apical tissues |
Occlusal |
25 Months |
Spontaneous pain, tenderness on percussion |
DPC #4 |
F/35 |
31 |
Reversible pulpitis |
Normal apical tissues |
Occlusal |
20 Months |
Spontaneous pain, fractured cusp |
PP #2 |
M/36 |
30 |
Reversible pulpitis |
Symptomatic apical periodontitis |
Interproximal |
12 Months |
Pulp Necrosis, tenderness on percussion |
Table 3 Demographic Data of Teeth with Unfavorable Outcomes
DPC, direct pulp capping; PP, partial pulpotomy
Analysis of predictive factors for pulp survival of VPT
The Cox regression was used to analyze the variables, including baseline demographic data and pre- and intra-operative factors (Table 4). Age, sex, pulpal diagnosis, presentation of pre-operative percussion tenderness, and pulp exposure type/location were not statistically related to the success of VPT (p > 0.05).
Variables |
p-value |
|---|---|
Age |
0.23 |
Sex |
0.6 |
Pulpal diagnosis |
0.97 |
Percussion |
0.97 |
Exposure type |
0.99 |
Exposure location |
0.94 |
Treatment |
0.09 |
Table 4 Predictive Factors for Pulp Survival of VPT Using Cox Regression
Discussion
This retrospective study investigated the outcome of VPT performed in the postgraduate endodontic clinic. To our knowledge, this is the first retrospective analysis of four types of VPT using BC-RRMFS and standardized protocol. As a relatively new material, the evaluation of BC-RRMFS is limited to a few in vitro studies9,11 and case reports.12 In the present study, we found that the success rate of each VPT group at 6 to 11 months was 100%. These results suggest the potential usefulness and biocompatibility of BC-RRMFS for VPT in permanent teeth.
The four groups of VPT in this study were homogenous in demographic data in terms of age, sex, tooth type, diagnosis, preoperative symptom, and type and location of pulp exposure. Many pulp exposures were caused by caries removal (IPC: 88.9%, DPC: 100%, FP:76.9%) except for the cases that received PP (50%). Furthermore, most of the treated teeth were molars in IPC, DPC, and FP. Interestingly, the proportion of anterior teeth and traumatic pulp exposure was higher in PP than in other procedure types. When the record about the period of pulp exposure after the trauma was accurate, PP was selected as the treatment of choice because of the predictable outcome.13 FP was performed automatically based on the standardized clinical protocol if bleeding control on exposed pulp tissue could not be achieved within 5-10 minutes. A recent study on VPT using other calcium silicates-based material reported the median exposure time. However, the specific correlation between exposure time and the success rate was not demonstrated.14 When mechanical or carious exposure interproximal or occlusal were compared, the groups were not statistically different, and the exposure type did not affect the pulp survival.
The condition of the pulp plays a decisive role in the outcome of conservative VPT. In a clinical setting, the determination of the proper status of the pulp is challenging for clinicians. The degree of pulpal bleeding upon pulp exposure is often considered a reflection of pulpal inflammation severity. Hemostasis that can be achieved in 5-10 minutes suggests that the pulp is not severely inflamed and VPT is predictable.15–16 However, studies using tricalcium silicate cement have shown that the time needed to achieve hemostasis did not significantly influence the treatment outcome.17–18 Instead, preoperative pain was determined a potential prognostic factor for unsuccessful outcomes requiring RCT.18 In this study, patients who presented a history of spontaneous and/or radiating pain were excluded. In addition, 57 teeth (80.3%) were diagnosed with reversible pulpitis, and 63 teeth (88.7%) were negative on preoperative percussion testing. Our results showed that pulpal diagnosis and presentation of percussion tenderness were not statistically related to the success of any VPT.
Three out of 66 treated patients returned with failure of treatment. Two failed cases confirmed spontaneous pain after an extended period of 20 - 25 months. However, the other failed case was asymptomatic. Furthermore, five asymptomatic patients returned to the endodontic clinic because of their general dentist’s request for RCT with restorative purpose, which shows the importance of communication between referrals. After additional discussion with patients and their general dentists, no need for RCT was accepted. Preoperative discussion about treatment plans with patients and referrals is necessary to reduce patients’ return after successful completion of VPT. The progress report about the case and request for follow-up appointments need to be provided to referrals promptly. In addition, our study included patients with ages ranging from 7 to 68 years, resulting in a mean age of 18.06 (±14.22) years. The failed cases have patient ages ranging from 24 to 36 years. Furthermore, a comprehensive review study reported that the success rate of VPT on carious pulp exposure is 92.4%.19 A recent study also revealed that the outcomes of pulpotomy in mature permanent teeth are approximately 90% up to 5 years, and age was not a significant factor in their outcome18. Therefore, endodontists should update their referrals on the VPT as a feasible definitive treatment in asymptomatic permanent teeth.
BC-RRMFS is a newly developed, ready-to-use calcium silicate-based bioactive ceramic material with excellent biocompatibility and sealing ability.11 It is premixed and induces less staining compared to MTA9 and has desirable handling properties and washout resistance.20 BC-RRMFS is quickly gaining popularity as VPT, perforation repair, and root-end filling materials because of these favorable properties. However, no clinical studies have shown the outcome of VPT treated with BC-RRMFS. In the present study, BC-RRMFS was used in all cases as the protective material for VPT, the cumulated proportion pulp surviving rates were 100% in IPC and 75% in PP over 18 months, and 75% in DPC and 95.5% in FP over 24 months. The result supports BC-RRMFS as the material of choice for VPT and the need for long-term studies.
The potential limitation of this retrospective study is recall bias. As a study based on retrospective chart review, one inherent limitation is selection bias. Because the data were mined from the existing database of patient recalls, it is difficult to determine whether successful or failed cases were more likely to return for follow-up appointments. Furthermore, this study was performed in the postgraduate students’ clinic of a dental school setting. The dental school environment and characteristics of referred patients may have influenced patients’ tendency to return for follow-up evaluations compared with a private practice environment. In addition, preoperative exam and recall notes were written by multiple different providers, which suggests slight variability in detail may be included in an individual’s treatment notes. Advanced dental education programs in Endodontics should encompass lectures in-depth and hands-on pieces of training with multiple materials about modern VPT. This curriculum will allow postgraduate students to master clinical skills in order to manage more challenging cases and achieve competence in VPT. Our findings revealed that high success rates in VPT can be achieved even by inexperienced clinicians with proper training.
Conclusion
Based on the results of this retrospective study, VPT with BC-RRMFS can be suitable for the management of carious and traumatic pulp exposure in permanent teeth. However, further long-term clinical studies with larger sample sizes are needed to provide a more definitive assessment of BC-RRMFS for VPT.
Acknowledgements
None.
Conflicts of Interest
None.
References
- Ricucci D, Siqueira JF, Li Y, et al. Vital pulp therapy: Histology and histobacteriology-based guidelines to treat teeth with deep caries and pulp exposure. J Dent. 2019;86:41–52.
- Swift EJ, Trope M, Ritter AV. Vital pulp therapy for the mature tooth – can it work? Endod Topics. 2003;5:49–56.
- Nyborg H. Capping of the pulp. The process involved and their outcome. A report of the follow-ups of a clinical series. Odontol Tidskr. 1958;64:296–364.
- Bjørndal L, Reit C, Bruun G, et al. Treatment of deep caries lesions in adults: Randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci. 2010;118:290–297.
- Nosrat IV, Nosrat CA. Reparative hard tissue formation following calcium hydroxide application after partial pulpotomy in cariously exposed pulps of permanent teeth. Int Endod J. 1998;31:221–226.
- Çaliskan MK. Pulpotomy of carious vital teeth with periapical involvement. Int Endod J. 1995;28:172–176.
- Mejàre I, Cvek M. Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol. 1993;9:238–242.
- Nair PN, Duncan HF, Pitt Ford TR, et al. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with Mineral Trioxide Aggregate: a randomized controlled trial. Int Endod J. 2009;41:128–150.
- Kohli MR, Yamaguchi M, Setzer FC, et al. Spectrophotometric analysis of coronal tooth discoloration induced by various bioceramic cements and other endodontic materials. J Endod. 2015;41:1862–1866.
- Ørstavik D, Kerekes K, Eriksen HM. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2:20–34.
- Miller AA, Takimoto K, Wealleans J, et al. Effect of 3 bioceramic materials on stem cells of the apical papilla proliferation and differentiation using a dentin disk model. J Endod. 2018;44:599–603.
- Sockalingam SNMP, Awang Talip MSAA, Zakaria ASI. Maturogenesis of an immature dens evaginatus nonvital premolar with an apically placed bioceramic material (EndoSequence Root Repair Material®): an unexpected finding. Case Rep Dent. 2018.
- Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1978;4:232–237.
- Haikal L, Ferraz Dos Santos B, et al. Biodentine pulpotomies on permanent traumatized teeth with complicated crown fractures. J Endod. 2020;46:1204–1209.
- Matsuo T, Nakanishi T, Shimizu H, et al. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod. 1996;22:551–556.
- Bogen G, Kim JS, Bakland LK. Direct pulp capping with mineral trioxide aggregate: an observational study. J Am Dent Assoc. 2008;139:305–315.
- Linsuwanont P, Wimonsutthikul K, Pothimoke U, et al. Treatment outcomes of mineral trioxide aggregate pulpotomy in vital permanent teeth with carious pulp exposure: the retrospective study. J Endod. 2017;43:225–230.
- Tan SY, Yu VSH, Lim KC, et al. Long-term pulpal and restorative outcomes of pulpotomy in mature permanent teeth. J Endod. 2020;46:383–390.
- Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod. 2011;37:581–587.
- Zhang W, Li Z, Peng B. Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. Int Endod J. 2010;43(9):769–774.