Volume : 1 | Issue : 1
Research
Implementing the evidence: Are call/recall systems for immunisations feasible in general practice?
Kerry Lonergan, Ali Latif , Thomas Beaney, Juliet Bailey, James Moore, Catherine Heffernan
London School of Hygiene and Tropical Medicine, England
Received: May 02, 2018 | Published: July 03, 2018
Abstract
Background: Patient invite-reminder systems (also known as call/recall) are one of the most cost effective ways to improve uptake of vaccination services. It is unknown how they are applied in routine practice in the UK. The aim of this study is to provide a cross-sectional description of the current situation in general practices across London and to provide insights into the facilitators and barriers to the use of call/recall.
Methods: Between October 2016 and February 2017 we undertook a census of all 1,301 London general practices. This was used as a purposive sampling frame for in-depth telephone interviews on experiences and perspectives on operating call/recall for immunisations.
Results: We had a 53% response rate with 684 general practices responding to the survey and 25 general practice managers volunteering to be interviewed. Over 85% of practices reported using a form of call/recall for childhood immunisations. Thematic analysis revealed call/recall was resource intensive and that letters and phone calls were considered better than text. Interviewees were aware of what ideal call/recall entailed but thought it was expensive. The majority felt call/recall belongs to general practice as they know their patients. Vaccinations were not seen as a priority for general practice.
Conclusions: This is the first study to describe how call/recall is utilized in day-to-day general practice in the UK. Delivery of call/recall varies widely, is resource intensive and is underutilised. Implementing best practice evidence to increase uptake and efficiency of call/recall processes will require investment and consorted effort.
Introduction
Vaccines are effective against a range of infectious diseases but suboptimal rates of immunisation continue to cause serious illness and deaths.1 Immunisation coverage is determined by a number of factors related to service provision, healthcare workers and individuals’ beliefs, knowledge and attitudes. Patient invite-reminder systems (also known as call/recall) are consistently cited as being one of the most cost-effective ways to improve uptake of vaccination services.2,3 By call/recall, we mean the process that healthcare providers utilise to systematically identify individuals eligible for immunisation, invite them to book or attend an appointment, remind them to attend and follow up those who have not attended or responded. Various systematic reviews4-9 have assessed the effectiveness of invite-reminder systems in improving immunisation coverage, with a recent Cochrane review estimating that it can increase uptake by 8%.10 While invite-reminders are ideally suited to individuals who may forget appointments, they also help encourage those individuals who may be more hesitant to take up an immunisation.11 Depending on how it is set up, an invite-reminder system can optimise uptake in a cost-effective manner. Using automated lower-cost methods (e.g. texts) for the whole population with more resource-heavy approaches for more defined cohorts (e.g. phone calls) can help strike the right balance between optimising uptake and minimising cost.12
To date, the body of evidence on the effectiveness of call/recall is USA based and it is unknown how this evidence is applied in UK general practices. In England, immunisation programmes are primarily provided by general practices. Immunisation services fall under additional services of the directly enhanced service component of the General Practice contract.13 General practices can opt out of providing immunisation services but not all programmes are contracted to utilise a call/recall system, for example the newer programmes of Shingles vaccine and Men ACWY to 19-25 year olds are offered opportunistically via an enhanced service, which practices choose to opt into.12 The aim of this study is to provide a cross-sectional description of what is currently happening in London general practices and to provide insights into the facilitators and barriers. This forms part of a larger NHS England (London) project to establish a best practice approach for proactive invites and reminders that would standardise service provision in London and assess changes to vaccination services uptake and immunisation coverage.
Methods
The study design was two-fold: (1) a survey to provide a cross-sectional description of call/recall systems in London GENERAL practices and (2) qualitative semi-structured interviews to gain further insight into the facilitators and barriers. Between October 2016 and February 2017 we undertook a census of all 1,301 London general practices. Practices were contacted by email with a link to an online questionnaire (appendix 1). Proactive invites and reactive reminders were defined and questions focused on which vaccinations had call/recall, what format the reminder took and who sent the reminder. The questionnaire was pretested by the NHS England (London) Immunisation Commissioning Team and piloted by three general practices. The revised tool was then forwarded to all practices using the NHS England (London) established email system. A reminder email was sent a week after the initial email, a second two weeks after that and a third three weeks after. We continued to contact non-responding practices until the end of January 2017, at which point, we believed no further responses would be obtained. Responses were imported into Excel 2010 and later into Stata version 14.2 for descriptive statistical analysis. We also divided the responses into those with call/recall and those without and imported practice descriptions such as practice population size, proportion of 0-4 year old children, deprivation score and 0-5 immunisation uptake rates as measured by 2nd dose of MMR. This latter variable was categorised into three (under 70%, 70-89%, 90% and over) reflecting the payment categories for vaccinations.14 Association between call/recall and continuous predictors was analysed using t-tests and for categorical predictors using Chi-squared tests. Two tailed t-tests were used, assuming equal variances.
The survey was used as a purposive sampling frame for in-depth interviews. Interviewees volunteered to be contacted for interview by providing their details at the end of the questionnaire. An interview schedule was used to guide the discussion, which allowed for flexibility and elaboration around each participant’s experience. This covered the following areas:
- Experiences of developing and implementing call/recall
- Knowledge of patient views on their call/recall system
- Perspectives on factors that facilitated service delivery
- Perspectives on challenges
- Views on improving call/recall across London
All interviews were conducted by two researchers (JB and AL) on telephone, in English and lasted approximately 30 minutes. Informed consent was obtained from each participant and pseudonyms were assigned to participants to protect identities. Interviews were audio-recorded, transcribed immediately and all transcripts were anonymised. Field notes were also made during the interview. The transcripts were read alongside the field notes to aid familiarisation and were analysed manually using the thematic analysis, with themes emerging from the data. Textual data were scrutinised for similarities and differences between themes. Issues that generated the most discussion were prioritised. Two researchers analysed the data separately to generate themes and then compared findings. Ethical approval was not required from National Health Services (NHS) as this was service improvement work.
Results
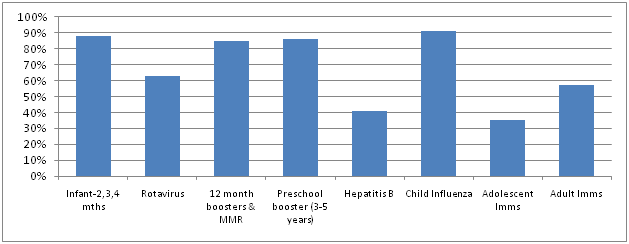
Responses were received from 684 general practices, providing a 53% response rate. Only 2% of general practices reported that they did not utilise call/recall systems. The majority of these practices use an invite reminder system for 0-5 routine childhood immunisations (Figure 1). This declined as age of child increased from 88% of practices reporting they invited parents for infant vaccines to 85% for preschool booster (usually given when child is aged between 3 years 4 months and 5 years). Practices reported separate invites for child influenza for 2,3 and 4 year olds (91%) and Rotavirus vaccine (65%), although the latter is part of the infant vaccine schedule. Infants born to Hepatitis B infected mothers should be actively invited for Hep B vaccinations yet only 41% of general practices reported doing this. Less than a quarter (23%), had an automated computer system for call/recall. Letters (81%) and telephone calls (80%) are the most popular methods for delivering invite-reminders with 65% using text-messages, 10% birthday cards and only 7% using emails. Once an invite has been sent, 75% of respondents sent follow-up reminders if an appointment has not been booked or if a patient/parent has not attended booked appointment (65%). Just under half send a reminder before a booked appointment. General practices reported that the main challenge to delivering call/recall was a lack of staff time (44%) with only 14% citing costs.
|
Figure 1 Proportion of London general practices that reported utilising a call/recall system by immunisation programme |
Practice description information was available for 617 practices, 572 of which used call/recall for at least one immunisation programme. No significant statistical association was found between call/recall and general practice population size (M=7399, t=-1.58, p=0.11), proportion of 0-4 year olds (M=6.5%, t=0.22, p=0.83) or deprivation (IMD15) score (M=24.3, t=-0.77, p=0.78). Those with MMR2 rates below 70% appear less likely to utilise call/recall (87.7% using call/recall) compared to the 70-89% using call/recall) and >90% (93.5% using call/recall). Number of reminders sent in those operating call/recall (once, twice or more than two reminders) showed no association with the proportion receiving the second dose of MMR.
Interviews
Twenty-five general practice representatives (practice managers) agreed to be interviewed and five represented single-handed practices. Three of these practices did not have a call/recall system; one of whom used health visitors to prompt. Five main themes emerged from the thematic analysis: (1) call/recall process varied by practice and was resource intensive; (2) letters and phone calls were considered better than texts; (3) awareness of the ideal call/recall; (4) preference to do it themselves and (5) vaccines are not a priority and patients aren’t bothered.
Call/recall process varied by practice and was resource intensive
The call/recall processes employed in practices and the interpretation of what constituted call/recall varied across interviewees. However, all had some elements of call/recall. Three had an IT system set up by their General Practice Federation which was automated, whilst another had their own bespoke system as “it was cheaper”. These systems routinely identified eligible cohorts and issued invites by letter. Texts were used to follow up on non-responses and if no further response, practice staff telephoned patients. The remaining 18 interviewees said they did call/recall manually. They identified the eligible parties through searches on their computer systems and sent invites as letters, texts or calling patients. They viewed automated systems as being expensive, requiring a lot of staff time, prone to error and not patient friendly. One interviewee from a single-handed practice (PM7) said that “they had no problems inviting in patients” so they didn’t need an automated system. Another (PM25) thought that as they;
“had a difficult population, we’re interested in setting up an IT system but don’t know if it could work with our multi-cultural and diverse population, particularly as language is a huge issue.”
Others said they distrusted the IT suppliers as being capable of doing call/recall. Even though it was time consuming, they liked to do it manually themselves. As a result, they didn’t do reminders routinely, but decided actions in accordance to the individual patient. There was also a focus on child immunisations with interviewees saying that apart from ‘flu vaccine, they didn’t have time for the other programmes.
Letters and phone calls are better than texts
Interviewees preferred to prompt patients with letters rather than texts or emails. As one interviewee (PM16) said:
“Letters may go to the wrong address but letters are more official, harder to ignore and often patients don’t have mobiles or change numbers or don’t like using texts. Patients are concerned about email and security. Some patients don’t have emails.”
Another interviewee (PM21) talked about not using texts as:
“you don’t know it is correct phone number, for example it may be for father and there may be child protection issues in using this mobile number, you can’t confirm who message is going to.”
Letters were also thought to be useful as many patients have little information. Two interviewees mentioned that in the past named health visitors made a difference as they spoke to parents about immunisations but now, parents rely on the letters for information and they wouldn’t be able to communicate this information in texts. Phone calls were typically used for reminders but two thought it better than letters as “people don’t open them” and when contacted “patients usually sound guilty on the phone” and more likely to come in (PM16). A single-handed practice interviewee (PM19) added:
“We have a high transient population so some get missed in that way but otherwise it is effective but is very costly in terms of phone bills and time spent by administrators. We have good vaccination rates and this is due to persistence by administrators. We also use all encounters - health visitor and nurse to remind about vaccinations, a noticeboard with immunisation schedule in the waiting room (this was after feedback from patients) and we have it on website and patients are often directed to website.”
How call/recall should look
Despite the variation in call/recall processes, all interviewees expressed awareness of what was needed to operate an efficient call/recall. Having a designated lead to co-ordinate the process was mentioned as was being flexible to optimise immunisation uptake. Three interviewees stated that this lead was their practice nurse. Flexibility, for the interviewees, encompassed using multiple methods and running immunisation clinics. All interviewees spoke of the importance of having a clear and simple-to-follow process that ensured that invite-reminders were sent out regularly and with minimal effort. This also ensured consistency even if different members of staff were involved. Two interviewees said that they implemented e-workflows that they felt made the process even more efficient. All spoke about practices normally have a good idea about how different groups or individuals respond to different invitations and reminders. Some require only reminding, others need direct calling from a practice nurse and others need even more encouragement. This is why they felt it was important to start early as identifying the eligible population in advance allows for invitation and booking in good time allowing greater focus on the more hesitant.
Preference to do it themselves
Twenty interviewees were adamant that call/recall was the domain of general practice. They expressed concern about loss of personal control, inaccuracies of addresses on centralised registries and “third party having access to patient identifiable information”. They also felt that tracking immunisation histories could not be done on centralised computerised systems as they would need to program immunisation algorithms to identify those eligible or overdue. This would be difficult as their patient populations move around a lot. One interviewee thought that centralising would duplicate their work, similar to what happened when a centralised cervical screening invite system was introduced. Invites from the practice was seen as being more personal and effective as they know their patients. The remaining five interviewees suggested that their General Practice Federations should implement centralised call/recall systems. They thought this would be beneficial in reducing costs and work burdens for individual practices and the system could link all parties that have responsibility promoting and providing vaccinations, e.g. health visiting services and school vaccination teams. Interestingly, none of the interviewees mentioned how Child Health Information Systems (CHIS) had operated centralised invite reminder systems for London borough populations in the past.
Vaccines not a priority and patients aren’t bothered
Vaccinations were not a priority on the list of primary care services that they needed to provide and “chasing patients” took up a lot of staff time. Resources were limited and they had other competing health service demands. For the three practices that did not have a call/recall system, the process was seen as being too difficult to implement and “cost heavy.” Call/recall for immunisations was seen as being time intensive and expensive for little return. They reported staff shortages and were limited in the number of vaccine appointments they could offer.
Six interviewees pointed out that from their experience, patients aren’t that interested in vaccinations and patients claim that they didn’t receive the texts or letters when asked. One interviewee (PM24) added that:
“in the past we have seen other practices use threat of removal saying they are worried they are a 'ghost patient' as way of getting patients in, I don’t agree with this.”
Instead, the receptionists are encouraged to opportunistically offer vaccinations when the patient books an appointment as “this gives ownership to the patient.”
Discussion
The majority of London based general practices have a form of call/recall system for immunisations in place, although the format varies by practice and by immunisation programme. Call/recall is more likely to be done for childhood immunisations with a lower proportion reporting call/recall for adult vaccinations (Figure 1), perhaps reflecting their long standing inclusion in the directly enhanced service of the GENERAL PRACTICE contract. The effectiveness of call/recall implemented in routine practice was also unclear. For example, 91% of practices report having call/recall for child influenza, yet this is the lowest uptake of all childhood immunisation programmes (30.3% vaccination uptake amongst 2 year olds, 32.6% amongst 3 year olds and 24.9% amongst 4 year olds in 2016/17).15 It is possible that doing call/recall in routine practice is affected by the appointment-based service which has been found to inhibit patient/parent behaviours around vaccinations.6,16
As the interviews illustrated, there was a preference to communicate personally with patients with letters or phone calls rather than use automated systems of letters, texts or emails. At the same time this personal investment was viewed as being time intensive for staff and costly to the practice. Interviewees were aware of what an effective call/recall system entailed but conveyed a gap between what was ideal and what was feasible. General practices provide a wide range of primary care services of which immunisation is a small component. Investing in effective call/recall was seen as requiring more effort than what vaccination services necessitated.
While the body of evidence has focused on the effectiveness of call/recall on improving vaccine uptake, there are some data on barriers and facilitators to its implementation. Similar to this study, financial and human resource constraints are the main impediments.4 Person-to-person telephone invites and reminders have been found by to be the most effective single approach,5,9 a mix of reminders being better than one approach9 and the timing of reminder having no effect on attendance.6 There is an emerging body of RCT evidence for text messages improving uptake of childhood immunisation appointments,17-19 including parents preferring texts to letters or phone calls17,20,21 and texts being the cheapest form of reminder.6 Evidence is lacking for emails,22 web-based and smart phone interventions,23 but there are studies underway looking at apps.24
Centralised call/recall systems with automated invites have been found in USA (and one London before-and-after study25) to be more effective than practice based systems in improving uptake of vaccination services.26-28 However, these studies have been conducted within research environments with financial investment and there is no clear indication of sustainability once implemented into mainstream service. None had long-term follow up with most analysing effectiveness at one year after the intervention. As this study shows, there is variation in call/recall processes across individual general practices but with common barriers of resources and staff capacity. Practices also liked ownership of call/recall. Any standardising of call/recall processes to improve immunisation uptake should be done collectively across groups of general practices, General Practice Federations or Alliances and CCGs. This can free up resource and ensure better equity for patients. The findings of this study can help instigate these collaborations.
Limitations of this study relate to selection and social desirability bias. It is possible that those who responded to the survey were more likely to have call/recall systems than those who did not. Those who engaged with the researchers are the same practices that interact regularly with the NHS England (London Region) public health commissioning team and so may be more familiar with immunisation updates and policies. Because this study was conducted on behalf of NHS England (London Region) public health commissioning team, respondents may have been reticent to fully disclose their problems with instigating call/recall particularly where they are contracted to do call/recall.
Conclusion
This is the first study to describe how call/recall for immunisations is utilized in day-to-day general practice in the UK. Delivery of call/recall is variable and not wide-spread. It is also costly and human and paper resource intensive. Implementing best practice evidence will require investment and consorted effort, in particular, promoting the use of automated computer processes using text invites and reminders.
References
- World Health Organisation. Global immunisation coverage in 2016.
- National Institute of Clinical Excellence. Immunisations: reducing differences in uptake in under-19s. NICE Public health guideline PH21. 2009.
- Jacob V, Chattodpadhyay S, Hopkins D, et al. Increasing coverage of appropriate vaccinations: a community guide systematic economic review. Am J Prev Med. 2016;50(6):797−808.
- Williams N, Woodward H, Majeed A, et al. Primary care strategies to improve childhood immunisation uptake in developed countries: systematic review. JRSM Short Rep. 2011;2(10): 81.
- Harvey H, Reissland N, Mason J. Parental reminder, recall and educational interventions to improve early childhood immunisation uptake: A systematic review and meta-analysis. Vaccine. 2015;33(25):2862−2880.
- McLean S, Gee M, Booth A, et al. Targeting the Use of Reminders and Notifications for Uptake by Populations (TURNUP): a systematic review and evidence synthesis. Health Services and Delivery Research. Southampton (UK): NIHR Journals Library; 2014.
- Pereira JA, Quach S, Heidebrecht CL, et al. Barriers to the use of reminder/recall interventions for immunizations: a systematic review. BMC Med Inform Decis Mak. 2012;12:145.
- Oyo-Ita A, Nwachukwu CE, Oringanje C, et al. Interventions for improving coverage of child immunisation in low- and middle-income countries. Cochrane Database Syst Rev. 2016;7:CD008145.
- Crocker-Buque T, Edelstein M, Mounier-Jack S. Interventions to reduce inequalities in vaccine uptake in children and adolescents aged <19 years: a systematic review. J Epidemiol Community Health. 2016.
- Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;3:CD003941.pub2.
- Betsch C, Böhm R, Chapman G. Using Behavioral Insights to Increase Vaccination Policy Effectiveness. Policy Insights from the Behavioral and Brain Sciences. 2015;2(1);61−73.
- Chachou M, Mukinda F, Motaze V, et al. Electronic and postal reminders for improving immunisation coverage in children: protocol for a systematic review and meta-analysis. Evidence Based Practice. 2015;5(10).
- https://www.england.nhs.uk/gp/gpfv/investment/gp-contract/.
- Specification for a directed enhanced service: Childhood immunisations.
- Seasonal flu vaccine uptake in GP patients in England: winter season 2016 to 2017. Public Health England.
- George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178−184.
- Hofstetter AM, Vargas CY, Kennedy A, et al. Parental and provider preferences and concerns regarding text message reminder/recall for early childhood vaccinations. Prev Med. 2013;57(2):75−80.
- Herrett E, Williamson E, van Staa T, et al. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open. 2016;6(2): e010069.
- Hofstetter AM, DuRivage N, Vargas CY, et al. Text message reminders for timely routine MMR vaccination: A randomized controlled trial. Vaccine. 2015;33(43):5741−5746.
- Clark SJ, Butchart A, Kennedy A, et al. Parents' experiences with and preferences for immunization reminder/recall technologies. Pediatrics. 2011;128(5): e1100−5.
- Ahlers-Schmidt CR, Chesser K, Paschal A, et al. Parent Opinions About Use of Text Messaging for Immunization Reminders. J Med Internet Res. 2012;14(3):e83.
- Atherton H, Sawmynaden P, Meyer B, et al. E-mail for the coordination of healthcare appointments and attendance reminders. Cochrane Database Syst Rev. 2012;8:CD007981.
- Odone A, Ferrari A, Spagnoli F, et al. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage. Hum Vaccin Immunother. 2015;11(1):72−82.
- Wilson K, Atkinson K, Pluscauskas M, et al. A mobile-phone immunization record in Ontario: uptake and opportunities for improving public health. J Telemed Telecare. 2014;20(8):476−480.
- Atchison C, Zvoc M, Balakrishnan R, et al. The evaluation of a standardized call/recall system for childhood immunizations in Wandsworth, England. J Community Health. 2013;38:581–587.
- Cockman Philippa, Dawson Luise, Mathur Rohini, et al. Improving MMR vaccination rates: herd immunity is a realistic goal. BMJ. 2011;343:d5703.
- Kempe A, Saville AW, Dickinson LM, et al. Collaborative centralized reminder/recall notification to increase immunization rates among young children: a comparative effectiveness trial. JAMA Pediatr. 2015;169(4):365−373.
- Szilagyi PG, Albertin C, Humiston SG, et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Acad Pediatr. 2013;13(3):204−213.